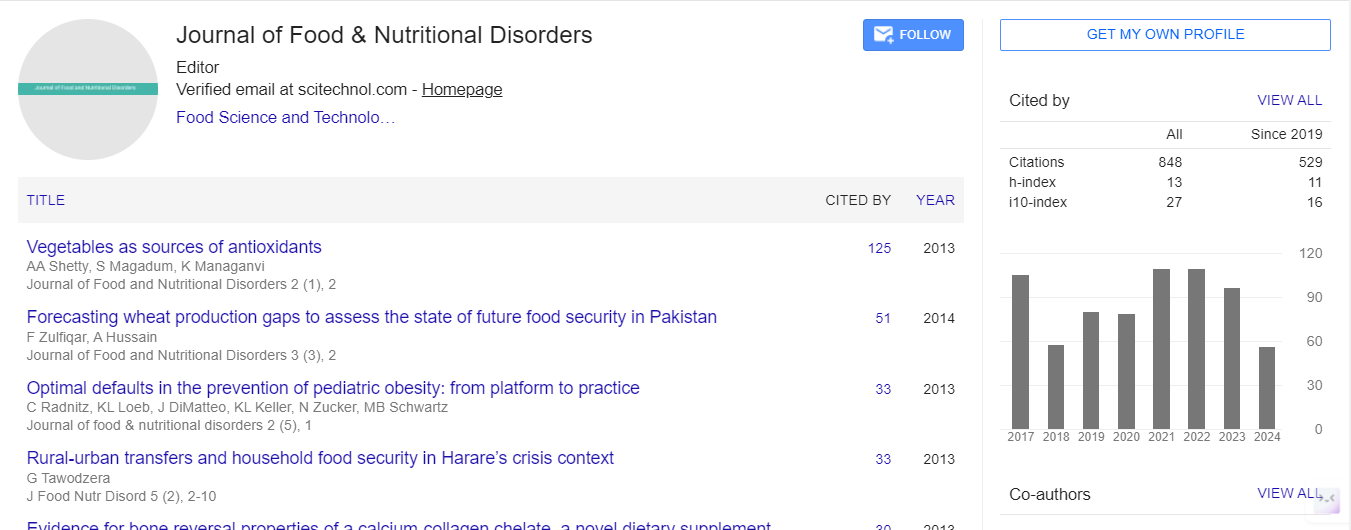
Research Article, J Food Nutr Disor Vol: 3 Issue: 4
Efficacy of a Minimal Dose School Fruit and Vegetable Snack Intervention
| Patti-Jean Naylor1*, Jennifer McConnell1, Ryan E. Rhodes1, Susan I Barr2, Isabella Ghement3 and Jenny Scott4 | |
| 1School of Exercise Science, Physical and Health Education, University of Victoria, Canada | |
| 2Food, Nutrition and Health, University of British Columbia, Canada | |
| 3Ghement Statistical Consulting Company Ltd., Canada | |
| 4Faculty of Health Sciences, Simon Fraser University, Canada | |
| Corresponding author : Naylor Patti-Jean School of Exercise Science, Physical and Health Education, University of Victoria. PO Box 3015 STN CSC, Victoria BC V8W 3P1, Canada Tel: 1(250) 721-7844; Fax: 1(250) 721-6601 E-mail: pjnaylor@uvic.ca |
|
| Received: March 10, 2014 Accepted: June 29, 2014 Published: July 02, 2014 | |
| Citation: Patti-Jean Naylor, Jennifer McConnell, Ryan E. Rhodes, Susan I Barr, Isabella Ghement, et al. (2014) Efficacy of a Minimal Dose School Fruit and Vegetable Snack Intervention. J Food Nutr Disor 3:4. doi:10.4172/2324-9323.1000147 |
Abstract
Efficacy of a Minimal Dose School Fruit and Vegetable Snack Intervention
Fruits and vegetables are important to health but the majority of Canadian children are not consuming enough of them. The provision of free fruit and vegetables at school over a school year significantly increases fruit and vegetable intake but the costs may prohibit adoption or sustained implementation of this approach. To address the issue of cost we evaluated the impact of a minimal dose free school fruit and vegetable snack intervention (4 months of intervention, 14 servings, 2 times/week every second week).
Keywords: Fruit; Vegetable; Snack; Dose; Minimal; School
Keywords |
|
| Fruit; Vegetable; Snack; Dose; Minimal; School | |
Introduction |
|
| Inadequate fruit and vegetable (FV) consumption has been associated with cardiovascular disease, type 2 diabetes (indirectly), hypertension, and cancer in adults [1-4]. Consumption during childhood may also be independently associated with burden of disease later in life as higher childhood vegetable intake has been associated with reduced stroke risk [5]. Fruit and vegetable consumption may also contribute to healthy weight trajectories by decreasing caloric density and consequently total caloric intake [2,3]. Unfortunately Canadian research has demonstrated that young Canadians are eating less than five servings of FV a day [6], a substantive proportion of those eating less than three [7], while the current Canadian guideline for 9-13 year olds is six servings/day [8]. Further compounding the issue is the evidence that lifestyle (including eating behaviors) may track from childhood through to adulthood [9-14]. Thus, increasing inadequate fruit and vegetable consumption during childhood may contribute to addressing escalating obesity and the development of chronic diseases across the lifespan [15-17]. | |
| Many interventions aimed at increasing fruit and vegetable consumption have been implemented in the school setting because schools provide equitable access and high levels of contact over time to promote health and well-being [18,19]. Free school fruit and vegetable snack interventions specifically may further reduce health inequalities by providing FV to children from low socioeconomic backgrounds. For instance, the Norwegian school fruit and vegetable scheme compared providing free FV to providing subsidized FV and found that the free scheme was taken up by all groups and the subsidized scheme was mainly taken up by those from a higher socioeconomic bracket [20]. In the free scheme differences in fruit and vegetable consumption between children across socioeconomic groups were reduced and sustained three years after the program [20,21]. | |
| Systematic reviews have shown that school fruit and vegetable interventions have a positive effect on fruit and vegetable consumption, although findings vary and effect sizes remain modest [19,22-26]. For instance ten of the fifteen (67%) school-based fruit and vegetable interventions reviewed by Knai et al. significantly increased fruit and vegetable FV consumption with the increase ranging from +. 3 - +.99 servings/day [19]. | |
| As evidence of the links between consumption and accessibility, availability and tasting experiences/exposures emerged in the literature [27-31] a more ‘environmental approach’ to school-based interventions was adopted whereby fruit and vegetable snacks were provided to students. We identified 13 studies (Table 1) that had provided children with fruit or FV during school hours; 12 provided these for free (one for part of the intervention period) [20,32-43]. | |
| Table 1: Summary of fruit and vegetable snack intervention studies | |
| Nine of the studies found significant increases at, or near half, a portion of FV a day [20,33,34,36,37,39,40,42,43]. Two found smaller significant increases of around one third of a FV portion per day [35,41] and a study from the Netherlands found that a free fruit or vegetable scheme and a multi-component program including free fruits or vegetables both significantly increased fruit or vegetable consumption by 0.20 portions per day [32]. A final study we reviewed did not report fruit and vegetable intake in portions but found significantly more (18.2%) intervention students reported eating fruit at least once a day compared to control group students [38]. In short, there was consistent evidence of the positive impact, albeit variable effect sizes, of school fruit and vegetable snack interventions. | |
| Some of the variability in the size of effects may arise from methodological differences across studies including design, measurement and the level of implementation or intervention dose (a combination of frequency and length of contact and intervention duration) [44]. Seven studies used randomized designs [20,32-34,40,41,43] and only seven controlled for the independent influence of cluster [20,32-35,41]. In terms of measurement, ten studies used a 24-hour recall to assess fruit and vegetable intake, eight used a range of food frequency questions and five used both (two studies employed trained personnel to conduct 24 hour recalls). Further, five used parent report of student intakes; seven used student report; and one both. Intake assessment ranged from multiple questionnaires [20,32,36,42,43] to a modest two questions about fruit intake only[34]. | |
| In looking more closely at the level of implementation or dose used in the 13 studies, nine provided daily fruits or vegetables [20,32-34,36-38,41,42] and four provided fruits or vegetables less than five times per week while maintaining statistically significant increases in fruit or vegetable consumption compared to comparison groups [35,39,40,43]. A study by Tak et al. used the most modest frequency. They provided fruits or vegetables twice a week over one school year and found an average difference of .23 pieces of fruit and approximately .17 servings of vegetables per day between the intervention group and comparison groups [35]. The only published Canadian study to date [40] served one piece of fruit or vegetable three times a week for 21 weeks. They found that the intervention group consumed 0.49 of a serving/day (p<0.05) more vegetables while at school than the comparison group. A study by Eriksen et al. applied the lowest total dose (n=25 deliveries) with FV provided at the highest frequency (daily) but for a shorter duration (five weeks). They found an average increase of 0.4 servings of fruit per school day in their intervention group [42]. To date programs have evaluated the impact of interventions varying from five weeks to two school years in duration and with a frequency of provision from two to five times per week. Fruit and vegetable snack programs provided a total dose ranging from a minimum of 25 to a maximum of 340 deliveries. | |
| Despite the variability in the interventions and findings, the weight of the evidence suggests that adopting fruit and vegetable snack programs leads to modest increases in intake that could have population health benefits. However, encouraging state, local, school district, or school level adoption and implementation of these types of initiatives may rely not only on evidence of effectiveness but more pragmatic information about cost which is directly affected by the dose of intervention needed to achieve meaningful change in addition to other factors such as supply, distribution mechanisms and geography. The cost or the cost-effectiveness of FV programs has not been addressed in the literature to date however, lower dose, less complex interventions are less costly (both in terms of time and financial resources) and thus theoretically are more conducive to adoption and implementation in the school system [45,46]. Thus there was a need to explore more minimal dose interventions and the British Columbia (BC) School Fruit and Vegetable Nutrition Program (SFVNP) provided us with the opportunity to do this. | |
| Based upon the consistent evidence from other jurisdictions and the promising results of a school fruit and vegetable snack pilot project [47], three BC government Ministries (Health, Education, Agriculture) came together with industry and non-government stakeholders to scale up the school fruit and vegetable program across the whole province [47]. To deal with issues of cost, supply and distribution the scale-able model provided local fruit and vegetable snacks to schools twice/week every second week. Schools applied for one of two intake periods, fall or winter and the winter term intake of new schools during the 4th year of scale-up afforded us with the opportunity to study the impact of this lower dose intervention over one term. | |
| We aimed to study the impact of a short-term delivery cycle (14 servings of produce; 7 varieties; approximately half of the SFVNP total dose of 32/school year) on the fruit and vegetable consumption, knowledge and self-efficacy [48] of older elementary school children in BC (Grades 5 and 6). We hypothesized that there would be positive changes in all of these variables as a result of the intervention. | |
Materials and Methods |
|
| Intervention | |
| The BC School Fruit and Vegetable Nutrition program had a number of features: 1) FV were delivered twice a week every two weeks, 2) a focus on providing locally grown (BC) produce, 3) facilitation by volunteer parents rather than school staff and 4) information for teachers to display and teach about local FV with associated information post cards to send home to parents (voluntary). The program is currently in its seventh year of scale-up and 1439 schools (82% of K-12 schools) and over 525,000 students are receiving products annually (http://sfvnp.ca/the-story.php). Just over 6.9 million servings of fruit produced by 637 BC growers were delivered to BC schools in the 2012-2013 school year [47]. | |
| Research design and sample | |
| We used a pre-post quasi-experimental design with matched comparison schools. As a natural experiment, our study team was not in control of the intervention nor which schools received the intervention [49]. The study was approved by the Human Research Ethics and Behavioral Research Ethics Boards at the Universities of Victoria (#08-05-149g) and British Columbia, respectively. | |
| Intervention schools (n=33) were randomly selected and recruited by our research team (by phone and faxed information package) from a pool of schools (n=82) that met the inclusion criteria of a) being situated in one of 16 consenting Districts, b) being registered to begin receiving the SFVNP produce during the winter term and c) not currently participating in any other health initiative (e.g. Action Schools! BC Healthy Eating [50] or Healthy Buddies [51]. We randomly selected 44 comparison schools from of pool of schools (n=298) that were a) located in the same School Districts (matched geographically, and b) not registered to participate and never having participated in the past in SFVNP or any other current health promotion initiative. Following recruitment efforts, 30% of the randomly selected SFVNP schools (10/33) and 28% of the comparison schools agreed to participate (10/44). | |
| After a school agreed to participate in the study, Grade 5 and 6 teachers were asked to send home an informed consent package. The signed consent was returned to the school by the student in a sealed envelope and collected by the research team. This yielded a sample of 773 consented Grade 5 and 6 children (10 - 12 years old), representing a 51% response rate; 61% in SFVNP schools and 41% in comparison schools. | |
| Procedures | |
| Data was collected from consenting students at baseline and followup by scheduling the class in the school’s computer lab. After baseline data collection, all children in the intervention schools began receiving deliveries from the SFVNP from February through May (4 months) at a frequency of two servings/week every second week; equalling a total of 14 servings. The control group carried on with usual practice. | |
| Measurement | |
| Descriptives | |
| We asked children about their gender and date of birth and calculated their age in years. We also assessed socioeconomic status by having them complete a previously validated Family Affluence Scale [52]. The affluence score (range 0-9) is computed from four questions that the children answer about family car ownership, holidays, household computers and bedrooms. For the purpose of this analysis (adjusting the model for this confounder) affluence was dichotomized to high (total score above 5) and low (total score 5 or lower). | |
| Children’s fruit and vegetable consumption | |
| We assessed children’s fruit and vegetable consumption before and after the intervention using two strategies that have been described in detail previously [53]. In short, children completed a validated and reliable web-based 24-hour food recall [54] about their food and beverage intake from the previous day and the Harvard Food Frequency Questionnaire for Children (FFQ-C) [55,56] to collect information from them about their consumption patterns over the last seven days. We focused on FV (together and separately) but also collected descriptive data about consumption of foods across the other main food groups and about the ‘other food’ category (which consists primarily of high-fat or high-sugar foods that are not considered to fall within the four main food groups). | |
| Children’s knowledge and self-efficacy | |
| To assess change in student knowledge of fruits and vegetables we asked children to indicate the FV (from a fixed list) that they knew were grown in BC (15 types) and not grown in BC (5 types) with the number of correct responses representing their score and higher scores representing more knowledge. To measure change in FV self-efficacy we used a psychosocial questionnaire adapted from the Gimme 5 study [57] that asked children about their level of agreement (on a 5 point likert scale) with 24 different efficacy statements (e.g. “For lunch at school, I think I can eat a vegetable that’s served” or “…eat carrot or celery sticks instead of chips”). Higher total scores (possible range from 24-120) represented higher self-efficacy | |
| Statistical Analysis | |
| Our statistical analyses were focused on the detection of intervention effects at follow-up for the following outcomes: (1) fruit and vegetable consumption a) during the previous 24 hours (also examining fruit only and vegetable only) and b) consumption during a typical week, (2) knowledge of produce grown and not grown in BC, (3) fruit and vegetable self-efficacy. Fruit and vegetables were measured in servings/day for the 24-hour recall and in servings/week for the FFQ-C. | |
| All statistical analyses relied on a Linear Mixed Effects Modeling framework in order to examine the intervention effects associated with the outcomes of interest at follow-up. We fitted four types of linear mixed effects models to the data for each of the outcomes. All four models included a fixed effect for group, which helped contrast the intervention and comparison groups, as well as a random effect for school nested within group. Furthermore, all models utilized the baseline value of the outcome as a covariate. The first and primary model did not include any additional covariates beside the baseline value of the outcome. The second model included one additional covariate, the change in calorie consumption between baseline and follow-up. The third model added another covariate – gender. The fourth model included all of the following covariates: calorie consumption, affluence level, total fruit and vegetable self-efficacy score and gender. All of the covariates were assumed to have fixed effects. We fitted only the first three types of linear mixed effects models described above to the data for the self-efficacy outcome because it was one of the covariates in the fourth model. For each of the four types of linear mixed effects models, the intervention effect was expressed as a difference in adjusted outcome means between the intervention and comparison groups, with the adjustment scheme being specific to each model and outcome. | |
| The analyses pursued here, commonly referred to in the literature as mixed effect ANCOVA, are considered a gold standard in research where randomization is by school and measurement is at the level of the individual [58]. The formal statistical analyses described above were supplemented by descriptive statistics of the distributions of the outcomes at interest at baseline and follow-up separately for the intervention group and comparison group, as well as for both groups combined. | |
| We conducted all of our analyses on the complete case data and performed a sensitivity analysis on the data for which the missing values were imputed in order to evaluate the reliability of our findings. The imputation of the missing data relied on the last observation carried forward approach and could only be performed for cases where the baseline value of a given outcome was available. For all statistical analyses, we set significance at p<.05. | |
| We conducted all statistical analyses using the statistical software package R [59]. More specifically, we used the lme() function available through the R package nlme. The primary focus of the analysis was fruit and vegetable consumption but we described intake from other food groups at baseline. | |
Results |
|
| Sample and baseline descriptive | |
| Six hundred and sixty-eight children (86% of consented children; mean age = 11.6, range 10.3 - 12.5 years old; 355 Girls; 312 Boys; Missing = 1) were present at school on the day of baseline data collection. Descriptive summaries of the baseline and follow-up levels of food group servings are shown in Table 2. | |
| Table 2: Descriptive statistics for food group servings of British Columbia school children in grades five and six that participated in the BC School Fruit and Vegetable Nutritional Program Evaluation, collected by self-report 24-hour recall at baseline and follow-up in the intervention and control groups. | |
| Children in this study were not consuming the amount of FV or dairy products recommended by the Canadian Food Guide [8] for their age group at baseline. However, the average intake for grain products and meat and alternatives at baseline was within guidelines. There were no significant group differences in consumption of FV or total calories at baseline regardless of the statistical adjustment scheme. The intervention group had a significantly higher knowledge of FV grown in BC score (adjusted mean difference = .77, SE=.03, p=. 02) and consumed more servings from the ‘other’ category at baseline when adjusting for clustering (Table 2). All further analyses were adjusted for baseline values. | |
| The intervention effects for the primary outcomes of interest after adjustment for baseline levels and school are displayed in Table 3 and specific analyses are highlighted in the following paragraphs. | |
| Table 3: Results of mixed linear effects modeling for select study outcomes based on the analysis of complete data adjusted for school and baseline values. Results include adjusted mean outcome values predicted via mixed linear effects modeling for intervention and control groups, the estimated intervention effect and the p-value for testing the statistical significance of the intervention effect. All reported adjusted means and differences in adjusted means are accompanied by standard errors. | |
| Children’s Fruit and Vegetable Consumption | |
| In analyzing fruit and vegetable consumption data after adjustment for school and baseline fruit and vegetable consumption, we found no significant difference at follow-up between the intervention and comparison groups in terms of average consumption of FV in the past 24 hours (Table 3). The analysis of the imputed data also showed no significant intervention effect. Additional analyses using the different adjustment schemes also failed to reveal any significant intervention effects for both complete case data and imputed data (results not shown). There were also no significant intervention effects found at follow-up for typical fruit and vegetable consumption (FFQ data) regardless of adjustment scheme. | |
| We also found no significant intervention effect at follow-up for fruit consumption alone or vegetable consumption alone as captured by the 24-hour recall after adjusting for school and baseline fruit consumption (Table 3). A secondary analysis performed using the imputed data also showed no intervention effect and there were no significant effects found for all other analyses or adjustment schemes (results not shown). | |
| Children’s Knowledge and Self-Efficacy | |
| We found no significant intervention effect at follow-up for knowledge of BC FV expressed as the number of correct responses to items that were grown in BC (Table 3) or the number of correct responses to items that were not grown in BC after adjusting for school and baseline knowledge. These findings were consistent with the imputed data analysis and regardless of adjustment scheme. | |
| We found no significant intervention effect at follow-up for total fruit and vegetable self-efficacy after adjusting for school and baseline fruit consumption (Table 3). Cronbach’s alpha for this scale was .941 and .942 for baseline and follow-up respectively. The analysis of the imputed data also found no significant intervention effect. | |
Discussion |
|
| There is a growing body of evidence from international [20,32-39,41-43] and Canadian [40] studies that free school fruit and vegetable snack schemes have a small but significant effect on children’s fruit and vegetable consumption over the short term. Experts have identified that there was a need to identify economically feasible models for sustaining FV initiatives for children and expanding their delivery to a broad population [60]. | |
| Considering the associated costs for these types of interventions, it is important to determine what dose is necessary to achieve the desired change in fruit and vegetable consumption. We had the opportunity to test a minimum dose intervention as a sub-study within an existing provincial school fruit and vegetable program. We implemented a ‘natural/real world’ comparison trial to determine if this ‘pared down’ intervention model (14 servings over 4 months) was efficacious. | |
| We found no significant intervention effects for students’ consumption of FV as measured by 24 hour recall or food frequency questionnaire, nor for knowledge of BC FV and fruit and vegetable self-efficacy when adjusting for cluster and known confounders at follow-up. Overall, these findings suggest that a lower dose of fruit and vegetable intervention (less frequent delivery and less total servings) didn’t have an impact. | |
| The results differ from the majority of the literature on fruit and vegetable schemes described earlier (Table 1). However, the BC SFVNP represented a substantive reduction in dose over other programs [14 servings versus a range from 25 -340 total servings] and over the closest comparable lower dose efficacious intervention (25 servings) [42]. In addition, because distribution costs to scale-up a program across a province spanning ~950,000 square kilometers needed to be considered, the frequency of delivery (twice every second week) was also lower than any other intervention (Table 1). Alternatively, the BC SFVNP program did include providing some educational information for teachers and parents about the locally grown FV being served, which could be seen as increasing the dose in terms of the intensity of the intervention. Unfortunately use of the materials was not assessed. | |
| Our results should be viewed in light of the known limitations of collecting self-report dietary behavior from children that has been consistently raised by other researchers [61,62]. We also conducted a natural experiment where schools were already registered in the program and although we attempted to recruit a random sample from each pool of schools the response rate at the school level was low. Thus there may have been some systematic bias introduced that could have influenced the results. We were also not able to differentiate between in- and out-of-school fruit and vegetable consumption. The Northern Ontario Fruit and Vegetable Scheme showed an impact on ‘in school’ consumption, but no impact on overall consumption [40]. On the other hand the strengths of our study include: the statistical analysis which adjusted for school-level effects, baseline differences and known confounders; utilizing two methods of assessing dietary consumption; and the naturalistic nature of the research design in that the intervention was conducted in ‘willing’ schools where implementation issues were less likely. | |
| In light of low levels of fruit and vegetable consumption among children [4,6]; their potential contribution to chronic disease prevention [4]; international evidence of the efficacy of free school fruit and vegetable interventions; and the importance of equitable exposure and access for children; fruit and vegetable snack interventions are a recommended component of a public health strategy to improve children’s diet. However, it appears that the number of servings and length of implementation matter. Our results showed clearly that 14 servings over 4 months accompanied by information for the teacher and parents was not effective. | |
Acknowledgements |
|
| We would like to acknowledge the funding provided by the Canadian Institutes of Health Research (GIR - 89051 PJN PI). We would also like to thank everyone in the schools that made The School Fruit and Vegetable Nutrition Program study possible including the principals, teachers, parents and children. We also appreciated the support offered by the BC Agriculture in the Classroom management team and by Professor Paul Veugelers and his team at the University of Alberta. As always this study wouldn’t have been possible without the commitment of the staff and students in the Chronic Disease Prevention and Knowledge Exchange Research Unit at The University of Victoria so we extend our heartfelt thanks. | |
References |
|
|
|
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi