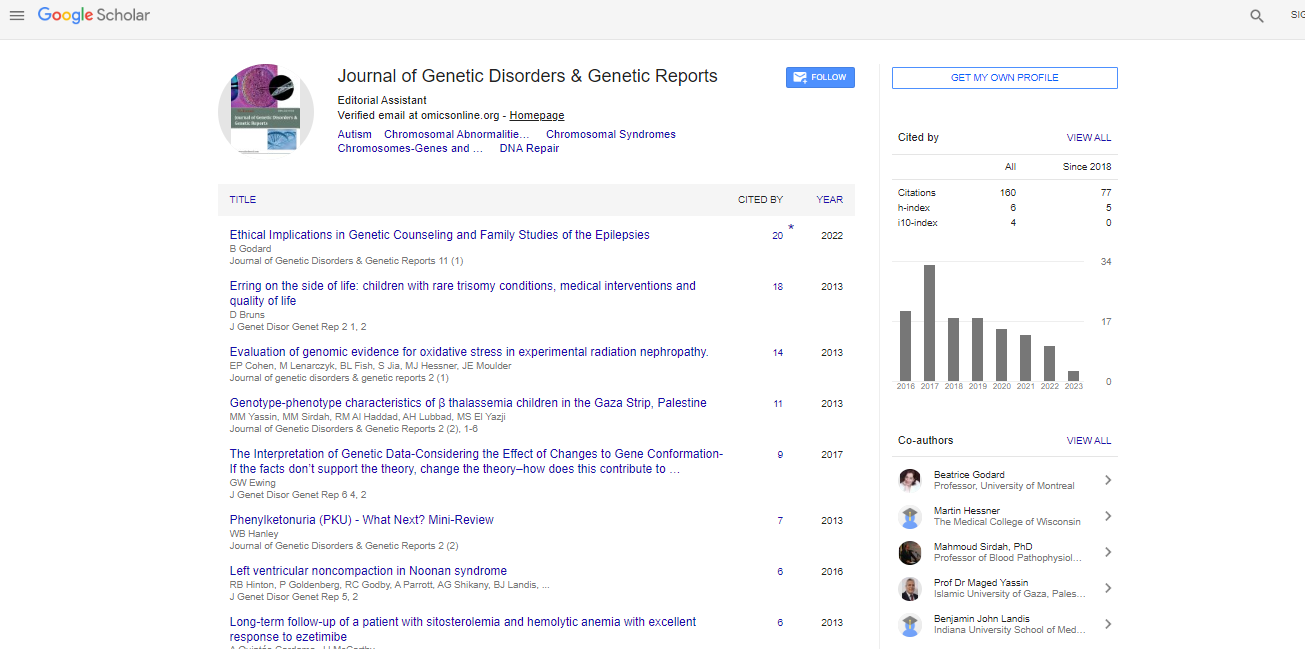
Case Report, J Genet Disor Genet Rep Vol: 7 Issue: 1
A case of Tuberous Sclerosis Complex Masquerading as Birt-Hogg-Dubé Syndrome
Kong YL1*, Oon HH2, Choudhury Y3,4 Tan MH2-4 and Ng SK1
1Department of Dermatology, National Skin Centre, Singapore
2Division of MedicalOncology, National Cancer Centre, Singapore
3Institute of Bioengineering and Nanotechnology, Singapore
4Lucence Diagnostics Pte Ltd, Republic of Singapore
*Corresponding Author : Kong YL
Department of Dermatology, National Skin Centre, Singapore-308205, Singapore
Tel: +(65) 91892550
E-mail: ylkong@nsc.com.sg
Received: April 03, 2018 Accepted: April 30, 2018 Published: May 07, 2018
Citation: Kong YL, Oon HH, Choudhury Y, Tan MH, Ng SK (2018) A Case of Tuberous Sclerosis Complex Masquerading as Birt-Hogg-Dube Syndrome. J Genet Disor Genet Rep 7:1. doi: 10.4172/2327-5790.1000169
Abstract
Tuberous sclerosis complex (TSC) and Birt-Hogg-Dubé syndrome (BHDS) act via the mammalian target of rapamycin (mTOR) pathway, resulting in overlapping clinical presentations. We report a patient who presented with features suggestive of BHDS: multiple fibrofolliculomas, a history of spontaneous pneumothorax and a positive family history of a renal condition. Subsequent genetic testing confirmed a Tuberous sclerosis complex 2 (TSC2) gene mutation, corresponding to a diagnosis of TSC. This case highlights how closely intertwined both conditions are, and also confirms that fibrofolliculomas are a feature of TSC.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi