Case Report, J Genet Disor Genet Rep Vol: 13 Issue: 1
A Typical Presentation of Ramsay Hunt Syndrome (RHS): A Case Report
Mahmoud Hussien Salih Daoud*, Abubakr Elmotesim Abdulla
Elamin, Abdelmuniem Ahmed, Mohmed Hussien Ahmed Mohmed
and Mohammed Hyder Hamid
Department of Medicine, University of Gezira, Wad Madani, Sudan
*Corresponding Author:Mahmoud Hussien Salih Daoud
Department of Medicine, University of Gezira, Wad Madani, Sudan
E-mail: dr.mhs.24@hotmail.com
Received date: 11 September, 2023, Manuscript No. JGDGR-23-113236;
Editor assigned date: 13 September, 2023, PreQC No. JGDGR-23-113236 (PQ);
Reviewed date: 27 September, 2023, QC No. JGDGR-23-113236;
Revised date: 09 January, 2024, Manuscript No. JGDGR-23-113236 (R);
Published date: 16 January, 2024, DOI: 10.4172/2327-5790.1000229
Citation: Daoud MHS, Elamin AEA, Ahmed A, Hamid MH, Mohmed MHA (2024) A Typical Presentation of Ramsay Hunt Syndrome (RHS): A Case Report. J Genet Disor Genet Rep 13:1.
Abstract
Background: Ramsay Hunt Syndrome (RHS) typically presents with a vesicular rash around the ear and facial paralysis. This case highlights an atypical presentation with rash distributed over cervical dermatomes.
Case presentation: A 55-year-old Sudanese woman presented with left-sided mouth deviation and difficulty closing her right eye following a vesicular rash on the right side of her head, ear, neck, and submandibular area. Initial misdiagnosis as dermatitis delayed appropriate treatment.
Conclusion: Awareness of atypical presentations of RHS is crucial for timely diagnosis and management. Early treatment with antivirals and corticosteroids significantly improves outcomes.
Keywords: Ramsay hunt syndrome; Cervical dermatomes; Atypical presentation
Introduction
Ramsay Hunt syndrome (also called herpes oticus) is a viral disease results from reactivation of varicella zoster virus in the geniculate body. Typically presented with paroxysmal pain deep within the ear, LMN facial nerve palsy with vesicular rash distributed around the anterior two thirds of the tongue, soft palate, external auditory canal, and pinna. Other cranial neuropathies might be affected and may involve Cranial Nerves (CNs) VIII, IX, X, V, and VI [1]. Without treatment, complete recovery occurs in about 20% of patients [2]. Combination treatment with antiviral and corticosteroid can improve outcome in RHS if started within 72 hours [3].
According to a prospective study conducted by Paul and Thiel, Ramsay Hunt Syndrome occurs at an incidence rate of 22.4/10,000 of the population [4].
This case highlights the coexistence of facial palsy with cervical dermatomal involvement as atypical presentation of RHS. The aim of this is to inform physicians about such kind of presentation of RHS in order to facilitate prompt diagnosis and appropriate treatment.
Ramsay Hunt Syndrome (RHS) results from the reactivation of the Varicella Zoster Virus (VZV) in the geniculate ganglion. Classic symptoms include ear pain, vesicular rash around the ear, and Lower Motor Neuron (LMN) facial nerve palsy. The condition may also involve other cranial nerves. Prompt treatment with antivirals and corticosteroids within 72 hours can significantly improve recovery rates. However, atypical presentations can complicate diagnosis and treatment.
Case Presentation
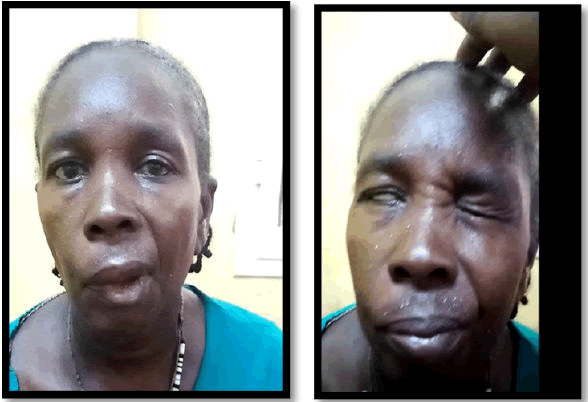
A 55-year old Sudanese female with a clear clinical background presented to Wad Medani teaching hospital with left side mouth deviation and difficulty in closure of her right eye. Two weeks earlier she complained of pain over the right side of her head, ear, and down to the right side of her neck, as well as submandibular area. Then she noticed a vesicular rash over the same area two days later. The patient sought medical advice and was diagnosed as dermatitis. Accordingly, she received topical medication and the vesicles erupted. Ten days from the rash appearance, the patient developed facial asymmetry [5]. On clinical examination revealed hyper pigmented skin over the right side of her neck, ear, and head and also right sided LMN facial nerve palsy grade 5 according to House-Brackmann facial grading system. Based on that, the patient was diagnosed with Ramsay-Hunt syndrome and received acyclovir 800 mg tablets, five times per day for 10 days, and methylprednisolone 500 mg infusion for 5 days followed by oral prednisolone (Figures 1 and 2).
Figure 1: Showed hyper pigmented skin over the right side of her neck, ear, and head.
Figure 2: Showed right sided facial nerve palsy grade 5 according to House-Brackmann facial grading system.
The patient was seen after 42 days of discharge and showed improvement with grade 3 facial palsy based on House-Brackmann facial grading system. Given the clinical presentation and history, the diagnosis of Ramsay Hunt syndrome was established. The patient was promptly started on antiviral therapy with oral acyclovir 800 mg, five times daily for 10 days [6]. Additionally, she received intravenous methylprednisolone 500 mg daily for 5 days, followed by a tapering course of oral prednisolone. Despite the initial delay in diagnosis and treatment, follow-up at 42 days post-discharge showed significant improvement:
• Reduction in facial asymmetry, with facial nerve palsy improving to grade 3 on the House-Brackmann scale.
• Resolution of the vesicular rash and associated pain.
The patient’s recovery underscores the importance of early recognition and treatment of Ramsay Hunt syndrome, particularly in atypical presentations where the rash may involve cervical dermatomes rather than the more classic auricular distribution.
Discussion
This case is presented with an unusual distribution of the rash which was involving cervical dermatomes (C3, C4). In comparison, Robert Steffen, et al. revealed a case of RHS involving the fifth, seventh, ninth and tenth cranial nerves, as well as the second and third cervical sensory roots or ganglia [7]. Also Kamil Kayayurt, et al., demonstrated atypical case of Ramsay Hunt syndrome in a 42-year-old male, with cervical nerve involvement [8]. Another case, by Mali Worme, et al., revealed a case of RHS in a 54 years old Caucasian woman with eruption of rash in the right C2-C4 dermatomes.
This atypical rash presentation may increase the risk of associated long-term nerve damage by delaying the diagnosis and consequently the management. This is exactly what happened to our case that initially was diagnosed with dermatitis until she developed facial palsy 10 days after the appearance of the rash.
The cornerstone of managing RHS is the early empirical use of oral antiviral drugs, namely acyclovir or valacyclovir, in combination with oral steroid to improve the rate of facial palsy. acyclovir used to be the drug of choice for patients of RHS; however, new generations of antiviral medications such as valacyclovir, famciclovir, penciclovir and brivudine are being preferred due to increasing resistance. Furthermore, a high dose of intravenous methylprednisolone found to be warranted for a successful treatment of facial nerve damage as a late treatment option.
We gave the patient 800 mg of oral acyclovir for 10 days and 500 mg of intravenous methylprednisolone for 5 days; followed by a short course of oral prednisolone 30 mg for additional 7 days. Then the patient was seen in our referral clinic 42 days post discharge date, her facial palsy has recovered from grade 5 to grade 3 based on Brackmann-house score. This outcome is consistent with that of the similar reported cases.
Conclusion
During pregnancy, the physiological, hormonal, and hemodynamic changes can significantly impact the cardiovascular system, leading to an increased incidence of arrhythmias. Sinus arrhythmia is the most frequent arrhythmia observed during pregnancy, followed by extrasystoles and paroxysmal supraventricular tachycardia. While more severe arrhythmias such as atrial fibrillation, ventricular fibrillation, and high-degree AV block are rare, they still present critical risks that require careful management.
Pregnancy can exacerbate preexisting arrhythmias, particularly in older women or those with Congenital Heart Disease (CHD). The management of arrhythmias during pregnancy requires a comprehensive, multidisciplinary approach that prioritizes maternal and fetal safety. This involves a careful selection of antiarrhythmic drugs, consideration of potential changes in drug pharmacokinetics, and a thorough evaluation of the patient's cardiovascular status.
For women with Structural Heart Disease (SHD), congenital heart disease, or inherited arrhythmia syndromes, preconception counseling and close monitoring throughout pregnancy are essential. In cases where fetal arrhythmias are detected, management strategies may include transplacental drug therapy and frequent monitoring to mitigate risks.
When cardiac interventions are necessary, such as synchronized cardio-version or catheter ablation, the benefits of controlling maternal arrhythmias must be weighed against the potential risks to the fetus. In particular, managing these conditions requires careful attention to anesthesia, especially in situations where hemodynamic instability is present.
Ultimately, the approach to arrhythmia management during pregnancy should be tailored to each patient's unique circumstances, with an emphasis on minimizing risks to both mother and fetus while ensuring optimal maternal cardiovascular health. This requires a collaborative, team-based approach involving specialists in cardiology, obstetrics, and pediatrics to achieve the best possible outcomes.
Physicians should be aware of typical and atypical presentations of RHS to facilitate prompt diagnosis and provide appropriate management. Early intervention with antivirals and corticosteroids has shown to significantly improve outcomes in these patients.
Key clinical message
Vesicular rash over cervical dermatomes should be considered as atypical presentation of RHS.
Strengths
Prompt diagnosis and management of this condition led to an excellent outcome in this patient.
Limitations
Polymerase Chain Reaction (PCR) for VZV was not done, because of limited resources in Sudan.
Consent for Publications
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflict of Interest
The authors declare that they have no competing interests.
Acknowledgment
Gratitude and appreciation for colleges in Wad Medani Teaching Hospital and Gezira Research Training Advocacy group for their help and support.
Author’s Contribution
Mahmoud Hussien Salih Daoud: Made the diagnosis of the condition.
Abubakr Elmotesim Abdulla Elamin: Assist in writing the abstract, background and discussion. Abdelmuniem Ahmed: Assist in writing the abstract, background and case presentation.
Mohammed Hyder hamid: Assist in writing the case presentation. Mohammed hussein: Assist in revision of the case report and referasing.
Funding
No funding available.
Data Availability
The data used to support the findings of this study are included within the article under references and cited throughout the body of the article with a corresponding reference in the reference list.
References
- Monsanto RD, Bittencourt AG, Bobato Neto NJ, Beilke SC, Lorenzetti FT, et al. (2016) Treatment and prognosis of facial palsy on Ramsay Hunt syndrome: Results based on a review of the literature. Int Arch Otorhinolaryngol 20: 394-400.
[Crossref] [Google Scholar] [PubMed]
- de Ru JA, van Benthem PP (2011) Combination therapy is preferable for patients with Ramsay Hunt syndrome. Otol Neurotol 32: 852-855.
[Crossref] [Google Scholar] [PubMed]
- Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, et al. (2007) Recommendations for the management of herpes zoster. Clin Infect Dis 44: S1-26.
[Crossref] [Google Scholar] [PubMed]
- Paul E, Thiel T (1996) Epidemiology of varicella zoster infection. Results of a prospective study in the Ansbach area. Hautarzt 47: 604-609.
[Crossref] [Google Scholar] [PubMed]
- Murakami S, Honda N, Mizobuchi M, Nakashiro Y, Hato N, et al. (1998) Rapid diagnosis of varicella zoster virus infection in acute facial palsy. Neurology 51: 1202-1205.
[Crossref] [Google Scholar] [PubMed]
- Steffen R, Selby G (1972) “Atypical” Ramsay Hunt syndrome. Med J Aust 227-230
[Crossref] [Google Scholar] [PubMed]
- Kayayurt K, Yavasi O, Bilir O, Ersunan G, Giakoup B (2014) A case of Ramsay Hunt syndrome with atypical presentation. Turk J Emerg Med 14:142-145.
[Crossref] [Google Scholar] [PubMed]
- Worme M, Chada R, Lavallee L (2013) An unexpected case of Ramsay Hunt syndrome: Case report and literature review. BMC Res Notes 6:1-5.
[Crossref] [Google Scholar] [PubMed]
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi