Research Article, J Food Nutr Disor Vol: 12 Issue: 1
Can we Say No to Obesity?
Tabinda Sattar*
Department of Chemical Sciences, University of Bahaudin Zakaraya, Multan, Pakistan
- *Corresponding Author:
- Tabinda Sattar
Department of Chemical Sciences,
University of Bahaudin Zakaraya,
Multan,
Pakistan,
Tel: 3336156485;
E-mail: tabindasattarahsan22@gmail.com
Received date: 10 June, 2021, Manuscript No. JFND-23-33530; Editor assigned date: 14 June, 2021, PreQC No. JFND-23-33530 (PQ); Reviewed date: 28 June, 2021, QC No. JFND-23-33530; Revised date: 31 January, 2023, Manuscript No. JFND-23-33530 (R); Published date: 28 February, 2023, DOI: 10.4172/2324-9323.1000336
Citation: Sattar T (2023) Can we Say No to Obesity? J Food Nutr Disor 12:1.
Abstract
The main objective of this review is to provide an overview of health problems due to obesity summarizes the evidence on the health benefits of having a normal weight body and discuss the physiological outcomes by which body might lead to improved health conditions. The terms “obesity and health”, “diseases caused by obesity”, “obesity an alarming issue worldwide” were searched on medline and pumed databases. A reduce and required body weight promotes and improves the health. Several lines of evidence also appear to promote that the physical activity, calories burn, exercises, daily walks, healthy and balanced diet may result in sustained body weights and consequently improvements in human health. Daily walk/ exercise, balanced diet and active lifestyles are hypothesized to influence the obesity a lot. At population levels, this phenomenon can provide multiple public health benefits due to promising non-pharmacological approaches.
Keywords: Obesity, Obesity isues, Obesity consequences, Healthful adaptations, Healthy life-styles
Introduction
Although a lot of information regarding obesity, its causes, effects and remedies are available to public; actually more than 200000 hits observed for internet search on the topic, “obesity and health”. Contrarily there is limited an up to date information for the evidencesbased knowledge that will support the recommendation for public health issues caused due to obesity. Different population formats are facing obesity globally since a long time. Various news articles, publications, blogs and nutritional recommendations are included in this critical issue. More than one thousands items including, nutrition books, food supplements, diet recommendations and activities related to the obesity and health issues have been reported by major online retailer’s lists. This globally discussed topic includes a lot of review articles during the last two decades [1]. A need for suggestive human evidences has supported vigorous clinical investigations especially related to the obesity and its health issues. This review summarizes the evidences of the health benefits of the active lifestyles, balanced diet and discusses the physiological basis upon which the health outcomes may be sustained and provides an overview of some healthful adaptations that are hypothesized to impact health outcomes (Table 1). The compelling evidences from rodent models and reviews have been focused and human intervention studies are also presented. In the context of health benefits of a smart, healthy body, evidences from some male and female rodent models were proved helpful. The point of interest related to this review is the changes in weight with the changing life styles, dietary patterns, consequently resulting in a health protection from major diseases. Concluding remarks of this review are that evidence-based information regarding reduction in obesity for improving human health along with the future issues that must be addressed globally [2].
| Healthful adaptations | Description | Short-term effects | Long term effects |
|---|---|---|---|
| Calories intakes=Calories burn | Enough | Reduced body weight, disease Prevention | Healthful smart body |
| Exercise | More | Reduced body weight | No cholesterol, no heart diseases |
| Daily walk | More | Reduced body weight | No more diabetes |
| Physical activity | More | Ideal body weight | No more diseases |
| Sleep | Enough | No weight gain | No depression |
| Prudent diet | More | Constant weight | Healthy body |
| Western food | Less | No weight gain | Health improvements |
| Glycemic food | Less | No weight gain | Health improvements |
| Mediterranean diet | More | Constant body weight | Health Improvements |
| Carbohydrate | Less | Healthy weight | No obesity |
| Proteins | More | Healthy body | No obesity |
| Red meat | Less | No stomach issues | Improved stomach working |
| Minimally processed food | More | No weight gain | No diseases |
| Highly processed food | Less | Better health | Less risk of cancer |
| Whole fruits | More | Reduced body weight | No weight gain |
| Fruit juices | Less | No weight gain | No obesity |
| Vegetables | More | Reduction in body weight | No overweighting |
| Whole grains | More | No obesity | Improves liver health |
| Plant oils | More | No overweighting | No heart diseases |
| Animal oils | Less | Improves health | No obesity |
| Mono-unsaturated fats | More | Improves heart health | No obesity |
| Poly-unsaturated fats | More | Improves heart health | No overweighting |
| Saturated fats | Less | No heart disease | No obesity |
| Sugary drinks | Less | No risk of diabetes | - |
| Alcoholic beverages | Less | Improves heart health | No overweighting |
| 2-3 Large meals | Less | Improves stomach | No weight gain |
| 4-5 Small meals | More | Improves gut health | No weight gain |
| Dietary fiber | More | Reduced stomach aches | Better health |
| Nuts | More | Improves brain health | Health improvements |
| Snacks | Less | Reduced body weight | No weight gain |
Table 1: Specific healthful adaptations hypothesized to impact health outcomes.
Materials and Methods
A brief background of the considerable literature regarding, reduction in obesity and its health effects in animal models is presented in order to provide a thorough look of the translational outcomes that has been described with reference to humans. The effect of life styles, dietary patterns, and dietary behavior has been elaborated for humans. Some interventions examining the effects of active life styles, balanced diets and dietary timings with reference to humans have been focused in this review. A medline search was performed by using pubmed regarding the terms “obesity and its health issues”, “obesity and diseases”, “lifestyles and obesity”, and “dietary patterns and obesity”. Relevant papers from the reference list and current reviews addressing the topic were culled. Three categories of inclusion criteria for human studies included, a) Randomized and non-Randomized studies, b) adult male and female participants, c) Biomarkers of obesity including changes in body weight related to changes in blood pressure, risk of diabetes, heart diseases and cancer. This review may not be treated as a formal review or meta-analysis providing only statistical data about obesity and its bio-markers. But this review provides a systemic view of the obesity related issues. The intervention studies including duration, sample composition and study designs are quite dissimilar and cannot be combined. Calories intakes and burn is a separate issue regarding obesity and its health effects so it is discussed using human observational data at the end of this review [3].
Human intervention studies
Studies based on 20 intervention trials has been described, supporting the efficacy of weight loss (non-obesity) on human health [4].
Active lifestyles
Lifestyles pattern have been encountered to influence greatly the body weights. Active life styles involve the life patterns in which the calories intake is balanced by the calories burn. In 2007, it was reviewed that this active life style can be proved as much effective as simple caloric restriction in reducing obesity-related body weight for managing the glucose and insulin concentrations. Total plasma and triglyceride concentrations and reduced inflammatory gene expression were detected in some rodent models of obesity [5].
The metabolic effects of active lifestyles have been explored in six intervention studies. Actually 10-30 normal weight and 10 overweight or obese adults were the range of samples used. Information about the physical activity levels of these participants is provided (Table 2). All these six studies reported significant weight loss depending upon physical activity levels. In one month study of active life styling, the participants experienced a mean 5% weight loss. As a result these participants also experienced a decrease in at least one glucoregulatory biomarker. Mixed results of lipid levels were detected in all studies. Improvements in obesity levels and consequently in high density lipoprotein cholesterol levels were resulted in all these studies. Significant improvements in inflammatory bio-markers were assessed in five out of six studies [6].
| Sample size | Participants | Dietary intervention | Duration | Weight change | Regulatory bio-markers | |||
|---|---|---|---|---|---|---|---|---|
| Fitness | FFA | CVD | Diabetes | |||||
| Adopted active life-styles (Physical activity/Exercise/Daily walk) | ||||||||
| 50M 50F | Obese, adults | Low carbohydrate | 1 Month: Daily walk, exercise | ↓ | SS fitness | NS FFA | TGs CVD |
NS glucose SS insulin |
| 15F | Overweight adults | Prudent | 15 Days: Only some physical activity | ↓ | SS Fitness | FFA |
NS CVD | Insulin |
| 10F 5M | Healthy weight adults | Western | 16 weeks: Almost No physical activity | ND | ND | SS FFA | SS CVD | ND |
| 15M 8F | Obese adults | 50% of usual intake and 50% low carbohydrate | 12 weeks, some physical activity | NS | Fitness | ND | NS CVD | NS insulin |
| 10M 10F | Overweight, adults | Low fats | 24 weeks, some physical activity | ↓ | ND | NS FFA | ND | NS insulin |
| 25M 20F | Young, overweight | Low glycemic | 4 weeks, strong physical activity | ↓ | SS fitness | NS FFA | TGs CVD |
NS glucose SS insulin |
| 23M 14F | Obese, adults | Low carbohydrate | 4 month, daily walk, exercise | ↓ | SS fitness | NS FFA | TGs CVD |
NS glucose SS insulin |
| 50M | Obese, adults | Low glycemic | 16 weeks, some physical Activity | ↓ | SS fitness | NS FFA | TGs CVD |
NS glucose SS insulin |
| 25F 50F | Overweight, adults | Low fats | 30 weeks, some physical activity | ↓ | NS FFA | TGs CVD |
SS glucose NS insulin |
|
| 17M 18F | Overweight, adults | Prudent | 15 weeks, some physical activity | ↓ | ↓ | NS FFA | NS CVD | ND |
| 25M 20F |
Overweight, adults | Western (including non-healthy food, junk food) | 16 weeks, some physical activity | ND | SS fitness | SS FFA | NS CVD | ND |
| 40 M | Overweight, adults | Low carbohydrate | 23 weeks, no physical activity | ND | SS fitness | ND | NS CVD | NS insulin |
| 45M 45F |
Overweight, adults | High fats | 14 weeks, no physical activity | ↓ | SS fitness | ND | SS CVD |
SS insulin SS glucose |
| 10M | Overweight, adults | High proteins | 20 weeks, no physical activity | ↑ | Fitness | FFA |
ND | SS glucose |
| 30M | Overweight, adults | High glycemic | 12 weeks, no physical activity | ND | Fitness | SS FFA | SS CVD | SS glucose NS insulin |
| 25M 50F |
Overweight, adults | Western | 3 weeks, some physical activity | ND | ND | SS FFA | SS CVD | SS glucose NS insulin |
| Adopted dietary behaviors | ||||||||
| 30F 10F |
Overweight, adults |
3-4 short meals, no nighttime eating | 21 weeks, some physical activity | ↓ | SS fitness | NS FFA | TGs CVD |
SS insulin |
| 50 | Obese, adults | 4-5 short meals, with nighttime eating | 15 weeks, no physical activity | ↑ | ND | NS FFA | SS CVD | SS glucose NS insulin |
| 40M | Overweight, adults | 2-3 Large meals, no meal at nighttime | 26 weeks, no physical activity | SS fitness | NS FFA | ND | NS glucose SS insulin |
|
| 50M 50F |
Normal weight, adults | 4-5 short meals, no meal at night | 30 weeks, some physical activity | ↓ | SS fitness | ND | TGs CVD |
|
| 20M 10F |
Obese, adults | 2 Large meals, without breakfast and with nighttime eating | 4 weeks, some physical activity | ND | SS FFA | SS CVD | SS glucose NS insulin | |
| 50M | Obese, adults | 3-4 short meals with nighttime eating | 45 weeks, extreme physical activity | ↓ | SS fitness | NS | NS CVD | NS glucose |
Table 2: Studies of different life styles, dietary patterns and dietary behaviors of interventions in humans that assessed metabolic biomarkers of fitness, diabetes and cardiovascular disease.
Five of these six studies enrolled were based on overweight and obese that resulted in substantial improvements not only in weight but also in some metabolic risk factors as well. Gray recently reported that the only one-month strong physical activity resulted in a 30% weight reduction in both men and women that is a caveat of this area of research. The main findings of these studies noted the participants experienced significant weight loss with perceived work performances. Although this significant regimen suggests the modest weight loss with physical activity but some reports of extreme physical activity especially in muscular pains or diseased conditions may not be a physical public health intervention [7].
Good dietary patterns
The dietary patterns generally specify that energy consumption is associated with energy intakes on a regularly scheduled dietary behavior. The term dietary patterns generally describe the eating behaviors rather than limited or not eating at all for some specific time periods. This type of dieting regimen may be the basis for some energy restricted diets like low glycemic and low carbohydrate diets. Although some results also reported from the popular 3:4 diet patterns which involved low energy diet in 3 days of a weak and taking unrestricted diet in rest of the weak. The impacts of modified dietary patterns were investigated in mice. Decreased visceral fats and leptin were reported in mice after some energy-restricted diets. Reduced adipocyte size and cell proliferation were also observed after restricted diet as demonstrated from the studies of the same research group [8].
Ten trials of samples sizes ranged from 10-200 were investigated for the effect of good dietary patterns over the overweight and obese adults. Duration of taking good dietary patterns ranged from 2-6 months. Statistically significant weight losses were reported in 8 out of 8 studies (100%). Significant decreases in insulin and glucose levels were found in all the participants. Also reduction in circulating LDL cholesterol or TG and several inflammatory bio-markers were found in all the participants [9]. Interestingly feelings of fullness and levels of PYY (peptide tyrosine tyrosine) in almost all participants decreased resulting in reduced weight.
The feelings related to reduced energy intakes along with some changes in gut peptide levels associated with hunger were also experienced in almost all participants. Some aspect of mood or other behavioral side effects in response to these specific dietary patterns may occur in some participants. Generally some feelings of cold, irritable, low energy or hunger were reported in a few participants that may be related with different immunity of them. However a mean improvement in mood and self-confidence including reductions in tension, anger, and fatigue were experienced in most of the participants due to reduction in weight [10].
While comparing the results of three of the nine trials summarized above, 25% energy restriction per day with significant weight loss were observed. A significantly reduced insulin concentrations and other inflammatory biomarkers were reported in two studies. Only two studies reported much weight losses where dietary patterns along with some physical activity were entertained as well. Also another 16-Week controlled weight trial found that the good dietary patterns along with some exercise protocols resulted a superior weight loss (mean loss 6.5%) as compared with adopting a dietary pattern or exercise alone (mean loss 3.2%) or exercise alone (mean loss 1.1%) [11].
The efficacy of good dietary patterns for the weight loss is discussed in several reviews and meta-analyses. The authors report that the continuous energy restriction and weight loss is resulted from the overall metabolic benefits of good dietary patterns. Furthermore modest and mixed effects on gluco-regulatory markers, lipids, and inflammatory markers resulted from the limited number of intervention trials suggest that these eating patterns result in weight loss [12].
Results and Discussion
Good dietary behaviors
Good dietary behaviors were investigated in some rodent models as reported in two recent publications. The result of all the studies of these rodent models comprise of the reduction in body weight, total cholesterol, TGs, glucose and improvements in insulin sensitivity. Due to excepted outcomes of good dietary behaviors on weight loss, these experiments were done on mice. An intervention strategy was utilized in female obese mice for the overall metabolic benefits of the good dietary behavior, which will prove translational to both men and women [13].
Research on good dietary behaviors in animals highlights the potential importance of synchronizing the diet timings with daily circadian rhythms. The mice got obesity and type-2 diabetes, when he was fed with High-Fat Diet (HFD) throughout the night and the day, disrupting the normal nocturnal feeding cycle. This increased net caloric intakes resulted in disrupted cardiac rhythms. Comparatively the mice that was fed two times with normal eating, consumed equivalent energy with no obesity and other diseased conditions. Good dietary behaviors are also effective as an intervention for the metabolic dysfunction and consequently the diet induced obesity [14].
The impacts of time restricted feeding in humans have been identified in four intervention trials. The net result of all these trials was the significant reduction in weight. Coherent results were obtained from the study on 40 overweight/obese males which were prescribed a 3-4 time normal meal per day. Significant weight loss along with reduction in inflammatory biomarkers was detected in these persons after a 26-weeks time. In another cross over study on 30 obese men, taking 2 long meals per day, no weight losses were found. No biomarkers were assessed [15].
One study reported 5% weight reduction in 40 men that were taking 3-meals properly on time with some physical activity as well. Taking breakfast or not-taking has long-term metabolic effects. No weight reduction reported in the men taking 2-meals, by skipping breakfast although having some physical activity. 10% weight reduced in persons in a 30 weeks period that were taking 4-5 short meals per day with some physical activity. Considerable changes in measurements of tension, depression, anger, vigor, fatigue, or confusion were also estimated in these candidates [16].
Although skipping one or two meals condition per day may lead to some weight loss, but resultantly the participants were hungrier after these meal breaks and with higher plasma levels of acetylated ghrelin compared with their levels on the day having 3-4 short meals. If the participants have less calories-intake in lunch and dinner hours, yet the insulin and post-lunch postprandial glucose leptin, and acetylated ghrelin levels were higher on the breakfast-free day [17].
In a 4-week trial studies, the participants experienced no weight change, glycemic control, lipids, or inflammatory markers for period with no breakfast meal. However the participants that were having breakfast and other short meals with some physical activity were found with weight loss along with improved metabolic profiles by restricting the availability of food to the normal nighttime feeding cycle. So this subsequently reduced the risk of obesity and obesity related conditions, such as chronic diseases, diabetes and nonalcoholic fatty liver disease. Some epidemiologic evidences also support the metabolic health benefits of aligning food intake with day time and avoiding it during night time [18].
Some epidemiological studies
According to various literature reports, the nighttime eating is associated with obesity and increased risks of diabetes, cardiovascular disease, and cancer (particularly breast cancer). Various observational studies focus upon the point that consuming most of your day’s food earlier in the day and taking less or no food in late evening and night time will surely lead towards low weight and improved health conditions. Every increased duration of nighttime fasting intervals will be associated with reduced risks of severe diseased conditions.
According to NHANES (National Health and Nutrition Examination Surveys), increased nighttime fasting intervals were found useful in breast cancer survivors in those who used to take in less than 30% of their daily calories after 5:00 PM [19].
Clinical outcomes of night time fast and reduced obesity are associated with reduced risk of several common chronic diseases. Although much data is not yet available However consuming more energy in early day time and lesser as the day is prolonged will surely prove helpful for weight loss. Prolonged night time fasting intervals not only reduces obesity but improves hormonal secretion patterns, physical coordination, and sleep as well [20].
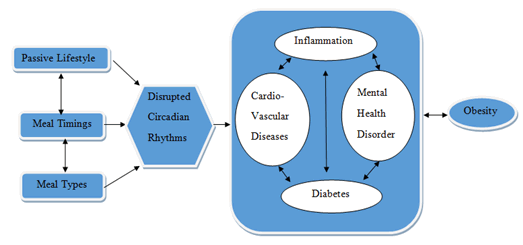
Obesity reducing mechanisms
A specific relationship among factors hypothesized to link reduced obesity risks with the health outcomes has been illustrated (Figure 1). Three important phenomena, a) circadian clocks, b) the gut microbiota, c) Specific life patterns can have great impacts on metabolic regulations of human body. A hostile metabolic milieu may be produced due to some negative perturbations of these biological and physiological systems. Resultantly the individuals facing these abnormalities may develop a predisposed can produce a hostile metabolic milieu, which predisposes individuals to increased obesity and other biomarkers of obesity cardiovascular disease, diabetes and cancer. Some recent and comprehensive reviews can well illustrate the potential linkage between obesity reducing mechanisms with health outcomes.
Circadian clocks
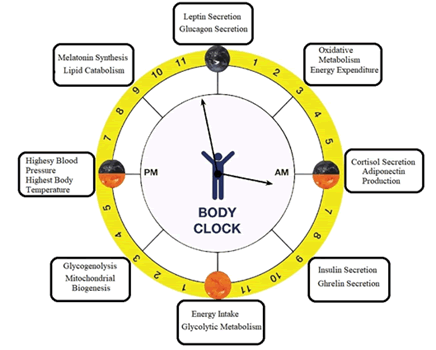
Nature has developed an endogenous circadian clock inside human body that is associated with day and night time. The physiological processes in organisms are performed at the optimal times accordingly with day and night (Figure 2). Human metabolism, energetic, as well as physiological indices are linked to light and dark stimuli which work according to the master biological clock situated in the suprachiasmatic nucleus of the hypothalamus and peripheral tissues, such as the liver, fat, and skeletal muscle cells. Across 24 hour light dark clock cycles, these circadian rhythms work with feeding as the dominant timing cue and includes changes in biology and behavior [21].
Circadian synchronizers i.e. nutrient signals and meal timing are interassociated that are disrupted by shift-work. Risk in cardio metabolic and other diseases may be increased due to the desynchronization of the suprachiasmatic nucleus master clock in the brain and peripheral circadian clocks in liver. Several metabolic pathways are controlled by the feeding signals that appear to be the dominant timing cue for the rhythms of peripheral clocks. Energy balances are disturbed by late-night eating in humans because of resetting of some peripheral clocks and thus consuming energy outside the normal feeding phase.
The suprachiasmatic nucleus in the hypothalamus serves as a “master clock” for brain and body. Normal brain functioning is according to circadian rhythms. The pineal gland situated in brain is responsible for the release of melatonin when it is darkness/night time. Any exposures to artificial lights will create difficulties in the release of melatonin and thus disturbances in your sleep cycle which will ultimately result in obesity. Due to circadian rhythms, another neurotransmitter, serotonin is released from brain in sunshine. Actually melatonin and serotonin are day and night hormones so any disturbance in your daily routine sleep-wake cycle will reset your circadian rhythms and will affect the whole body. Reduction in energy intake in evening and excluding energy intake during the nighttime will synchronize food ingestion with the times of optimal postprandial hormonal response. So any nighttime eating will affect the release of melatonin and it is hypothesized that time-restricted feeding regimens that actively impose a diurnal rhythm of food intake aligned with the 24-hour light dark cycle lead to improved sleep and health conditions as well.
Postprandial responses to meals increase across the day in humans due to the release of hunger hormone, gherlin from stomach. Basically the function of gherlin is to produce hunger feelings in several reports suggest that release of melatonin can cease the gherlin release. So human metabolism will be strongly affected by circadian rhythms across the day and night. Awaking late at night or exposure to artificial lights will disturb the circadian clock by decreasing melatonin secretions that will have metabolic consequences to perturb gherlin secretions. Thus hunger feelings late at night will induce misalignment in circadian rhythms in humans by extending the day. Resultantly late night food intakes and absence of sleep will cause obesity and type-2 diabetes. Leptin synthesis from liver is dramatically reduced by energy intake during the nighttime that will synchronize food ingestion with the times of optimal postprandial hormonal response [22].
Short-term intervention studies designed the circadian rhythms of insulin secretion that decreases through-out the day and into the night. The greater postprandial glucose and insulin exposure will occur to the meals taken after evening or late at night. Due to less sensitivity of insulin the meals consumed at night are associated with increased obesity, HbA1c levels and risk of type 2-diabetes over time than content-matched meals consumed during the day. Less or time restricted feeding after evening will make a proper secretion of another hormone, glucagon from pancreas that function as a circadian rhythm synchronizer for energy balances in body. Absence of melatonin also dramatically reduces glucagon levels that actively impose a diurnal rhythm of food intake leading to improved health. The improved body weight regulations are highly dependent over the oscillations in circadian clock gene expressions. So all these research studies strongly agree upon the fact that the improved human health and low disease risk is determined by the timing of food intake.
Gastrointestinal (gut microbiota
A very complex, diverse and vast microbial community resides in the human intestinal tract that will definitely affect the circadian, or sleep wake, rhythms of the gastrointestinal tract. The gut microbiome is exhibiting daily cyclical fluctuations in compositional diversity as it depends upon both the type and time of diet intake. Any disturbed circadian rhythms of gastrointestinal track would directly develop a mechanism by which the gut microbiome affects host metabolism. As the gastric emptying and blood-flow are greater during the daytime than at night so any disturbances in these normal circadian rhythms will affect the gut microflora. On the other hand the metabolic responses to a glucose load are slower in the evening than in the morning so a high glucose diet taken after evening will result in cyclical microbiota fluctuations. Further in obese individuals the net energy absorption, expenditure, and storage is highly influenced by their obese microbiota which may harvest more energy from the diet than a lean microbiota. Host circadian-metabolic axis, such as light/ dark cycles, sleep/wake cycles, diet, and eating patterns impact greatly upon the gut microbiota. With respect to composition, their localization to intestinal niches and functions, gut bacteria possess their own daily rhythmicity. There are some microbial metabolites such as butyrate, poly-phenolic derivatives, vitamins, and amines through which the gut bacteria would modulate host rhythms. Hence an altered sleep and eating patterns may influence the gut microbiota due to disturbance in the host circadian system. The substrate oxidation and energy regulation in the host are affected by the consequent disruptions to microbiota-mediated functions and would result in a decreased conjugation of bile acids or increased production of hydrogen sulfide with a decreased production of butyrate. Thus, insufficient sleep and circadian misalignment will at least partially contribute to an increased risk of obesity and metabolic syndrome due to disturbances in microbiome rhythms. For the maintenance of the gut microbial balances, essentially good sleep and a healthy diet must be required [23].
The host circadian rhythms and metabolic homeorhesis would be consolidated by activity of gut microbial abundance with manipulating daily rhythms for a promising chrononutrition-based approach. The gastrointestinal function of gut microbiome may impair metabolism and health of host because of its dynamic nature. According to some rodent studies it would be plausible that a chronically disturbed circadian profile may affect the gut microbiome, leading diet-induced obesity. Jet-lag and other metabolic imbalances can break a brain-gut pathway normally activated in the brain that acts to promote energy balances of body. Finally good life patterns and behaviors have positive impacts on human macrobiotic. Still important contributions to the field have to be made regarding the health impacts of obesity on human microbiota.
Some other life patterns
Energy intake and energy expenditure: Several life patterns impact greatly upon the human health and weight. According to some reports if nightly fasting was increased from twelve to fourteen hours, it results not only in improvements in self-reported sleep satisfaction, satiety at bedtime and energy levels, but also statistically significant decreases in energy intake and weight.
Decreased energy consumption was documented by both, the good dietary patterns and behaviors. Randomized controlled, weight loss trials based on breakfast skipping and eating lead to the evidences that obesity and obesity-related issues were due to low or no caloric intake in morning and more caloric intake in lunch or post-lunch hours. In a 3-day controlled trial study, more caloric intake in breakfast showed approximately 30% overall reduced caloric intake following a 75% calorie restriction in the whole day. Prolonged morning fast may lead to increased lunch and post-lunch appetite resulting in more caloric intake than was required in a proper 3-4 times proper meals timings. Shift or night workers, taking most of their calories in late evening or night hours were facing irregularities in appetite-regulating hormones so leading towards an increased caloric intake and obesity. Weight control and energy efficiency, both are controlled by the food intakes with respect to the timing of food intake in the 24-hour light-dark cycle [24].
As energy regulation and metabolism are controlled by our endogenous circadian system which impacts upon all the physiological processes in the body. As already described that obesity or weight gain may be caused due to energy consumption in late evening or night hours. So the two things, “when and what” we eat become important for the maintenance of energy balances of our body. So for a healthy body weight, energy intake to earlier during the day must be preferred. Some tightly controlled acute studies suggest that the energy expenditure typically more efficient earlier during the day either the body is at rest (resting metabolic rate) and after eating (thermic effect of food). While regarding energy utilization and balance of body, the key evidence for a circadian pattern is actually the meal intake timings. Further appropriate methodologies are required considering the role of meal timing for improving metabolic health and energy balance, while focusing on meal timing and frequency.
Sleep
A reduced sleep duration and poor sleep quality have been reported by nighttime eating as has been reported in numerous observational studies. As a result of this disrupted sleep pattern, the risks of obesity, diabetes, cardiovascular disease, and cancer may be increased a lot. Contrarily, a reduced risk of cardiometabolic disease and cancer has been elucidated due to prolonged nightly fasting on energy intake, sleep, physical activity, and circadian activity rhythm.
With a multiple risk factors and several complex mechanisms involved, there is an increased risk of prevalence of obesity worldwide. A regularized metabolism is only possible through the modulated circadian rhythms by enhancing certain energetic activities during day and night. Usually the energy metabolism is modulated by the circadian system, so a regularized metabolism of a body is dependent upon the regular circadian rhythms as described in some emerging evidences. Some emerging evidences indicated that sometimes circadian disruptions resulted from different lifestyles would result in modifiable risk factors causing sleep and metabolic disorders, finally ending up with increased obesity risks. The main role in the development of obesity would be contributed by the sleep disruption caused due to the circadian misalignment [25].
Illness and medication
Generally speaking obesity causes a lot of diseases like diabetes, high blood pressure obesity associated cardiovascular disease such as heart disease, gallstones, and other chronic illnesses. Contrarily some diseased conditions may cause obesity. Cushing's syndrome, hypothyroidism, insulin resistance and polycystic ovary syndrome are great contributors to obesity. Another disease, Prader-Willi syndrome has also been reported to cause obesity.
In addition to diseases, sometimes medication to cure certain diseases will also add to obesity. Such a condition will prove good for underweight or normal weight people. But already over-weight people will face difficult to manage an addition of few ponds to their weight. So weight-gain due to medications will be greatly dependent over the medical conditions, age and specific medicine. Tendency of weight gain might be different in different individuals, so taking medicines for months or years might be responsible for a lot of weight gain with 10 or 20 pounds in a few months. In this respect some steroid medicines are well-known for quickly weight gaining. Additionally some medicines of depression and schizophrenia cause weight-gain both in male and female of all ages.
Heredity
Some obesity cases were reported due to the rare single-gene defects causing extremely high levels of hunger and resulting in childhood obesity. Genetically some Leptin, POMC and MC4R deficiencies may be resulted in children before the age of 2 resulting in severe obesity. Increased hunger levels, increased caloric intake, reduced satiety, and reduced control over eating, increased tendency to be sedentary and store body fats are caused in some individuals due to the fat mass or obesity-associated gene.
Psychological and social factors
Conditions like anxiety, depression or even an eating disorder would be resulted in people with negative thinking, with struggling mental health, poor emotional management and low self-worth. As a consequence, conditions such as poor self-care, emotional overeating and little interest in regular exercise would be developed in those. Additionally sometimes, low self-worth, self-criticism, avoidance of emotions negative core beliefs and binge eating may result in sustainable obesity. For helping these critical situations, Cognitive- Behavioural Strategies (CBT) would proved as much effective giving an improved sense of healthier mindset, change in eating and exercise behavior thus reducing obesity [26].
Conclusion
Basal concentration of many metabolic biomarkers including chronic diseases are reduced by adopting active life styles, good dietary patterns and even good dietary behaviors as well. For promoting a better metabolic health, a regular physical activity with good dietary pattern and behavior would be proved a feasible and sustainable population-based strategy. Still more widely clinical research would be required for achieving steady-state controlled levels for many metabolic substrates and hormones for treatment of patients with extreme obesity conditions. More investigations are prerequisite to reveal the facts that long-term metabolic improvements and body weight management could be achieved by replacing energy restriction by proper food intakes. The current evidence supports the concluding Points. Practical eating patterns in rodents and other mammals translates the positive effects of better feeding regimens for reducing the risk of chronic disease in humans. Some other issues associated with observational research of obesity and human metabolic health has been discussed in future issues section. Losing weight for improving metabolic health is the main focus of this study especially for those people who can safely manage their diet with some physical activity by following circadian clock. Multiple public health benefits would be resulted at the population level only by following these simple approaches discussed in this overview.
References
- Al-Hazzaa M, Abahussain NA, Qahwaji DM, Musaiger AO (2012) Lifestyle factors associated with overweight and obesity among Saudi adolescents. BMC Pub Health 12: 354.
[Crossref] [Google Scholar] [PubMed]
- Sven A, Schroeter C (2017) The impact of nutritional supplement intake on diet behavior and obesity outcomes. PLoS One 12: e0185258.
[Crossref] [Google Scholar] [PubMed]
- Appel LJ, Moore TJ, Obarzanek E (1997) A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336: 1117-1124.
- Ball K, Crawford D, Mishra G (2006) Socio-economic inequalities in women’s fruit and vegetable intakes: A multilevel study of individual, social and environmental mediators. Pub Health Nutr 9: 623-630.
- Beck KL, Kruger R, Conlon CA (2012) The relativevalidity and reproducibility of an iron food frequency questionnaire foridentifyingiron-relateddietary patterns in young women. J Acad Nutr Diet 112: 1177-87.
[Crossref] [Google Scholar] [PubMed]
- Bleich SN, Vercammen KA, Zatz LY (2018) Interventions to prevent global childhood overweight and obesity: A systematic review. Lan Dia End 6: 332-346. [Crossref]
[Google Scholar] [PubMed]
- Bouchard-Mercier A, Paradis AM, Godin G (2010) Associations between dietary patterns and ldl peak particle diameter: A crosssectional study. J Am Coll Nutr 29: 630-637.
[Crossref] [Google Scholar] [PubMed]
- Bouche C, Rizkalla SW, Luo J (2002) Five-week, low-glycemic index diet decreases total fat mass and improves plasma lipid profile in moderately overweight nondiabetic men. Dia Care 25: 822-828.
[Crossref] [Google Scholar] [PubMed]
- Chan R, Chan D, Lau W (2014) A cross sectional study to examine the association between dietary patterns and risk of overweight and obesity in Hong Kong Chinese adolescents aged 10-12 years. J Am Coll Nutr 33: 450-458.
[Crossref] [Google Scholar] [PubMed]
- Chan SM, Woo J (2010) Prevention of overweight and obesity: How effective is the current public health approach. Int J Environ Res Pub Health 7: 765-783.
[Crossref] [Google Scholar] [PubMed]
- Pourazad M, Moussavi Z, Farahmand F, Ward R (2005) Heart sounds separation from lung sounds using independent component analysis. Conf Proc IEEE Eng Med Biol Soc 3: 2736-2739.
[Crossref] [Google Scholar] [PubMed]
- Lehner RJ, Rangayyan RM (1987) A three channel microcomputer system for segmentation and characterization of the phonocardiogram. IEEE Trans Biomed Eng 34: 485-489.
[Crossref] [Google Scholar] [PubMed]
- Sepehri AA., Gharehbaghi A, Dutoit T (2010) A novel method for pediatric heart sound segmentation without using the ECG. Comp Method Prog Biomed 99: 43-48.
[Crossref] [Google Scholar] [PubMed]
- Vivek N, Roland P (2005) Accessing heart dynamics to estimate durations of heart sounds. IOP Publ Ltd Physiol Meas 26: 1005-1018.
[Crossref] [Google Scholar] [PubMed]
- HAMZA CHERIF L, Debbal SM, Bereksi-Reguig F (2008) Segmentation of heart sounds and heart murmurs. J Mech Med Biol 8: 549-59.
- Zhihai Tu, Guitao Cao (2010) Improved methods for detecting main components of heart sounds. Six Int Conf Natural Comput Shang Dong Yantai.
- Hu XJ, Zhang JW, Cao GT, Zhu HH, Li Hao (2011) Feature extraction and choice in pcg based on hilbert transfer. 4th Int Cong Image Signal Proces (IEEE) 4: 2159-2163.
- Hamza CL, Debbal M (2013) Algorithm for detection of the S1 and S2 split and extraction of their internal components using a Hilbert transform. J Med Eng Technol 37: 220-230.
[Crossref] [Google scholar] [PubMed]
- Lehner RJ, Rangayyan RM (1987) A three-channel microcomputer system for segmentation and characterization of the phonocardiogram. IEEE Trans Biomed Eng 34: 485-489.
[Crossref] [Google Scholar] [PubMed]
- Groch MW, Domnanovich JR, Erwin WD (1992) A new heart sounds gating device for medical imaging. IEEE Trans Biomed Eng 39: 307-310.
[Crossref] [Google Scholar] [PubMed]
- Huiying L, Sakari L, Liro H (1997) A heart sound segmentation using wavelet decomposition and reconstruction. Proceed 19th Annual Int Confer IEEE-EMBS, Chicago, pp. 1630-1633.
- Sarkady AA, Clarck RR, Williams R (1976) Computer analysis techniques for phonocardiogram diagnosis. Comput Biomed Res 9: 349-63.
[Crossref] [Google Scholar] [PubMed]
- Atbi S, Debbal M, Meziani F, Meziane A (2013) Separation of heart sounds and heart murmurs by Hilbert transform Envelogram. J Med Eng Technol 37: 375-387.
[Crossref] [Google Scholar] [PubMed]
- Liang H, Lukkarinen S, Hartimo I (1997) A boundary modification method for heart sound segmentation algorithm. Comp Cardiol 25: 593-595.
- L. Hamza Cherif (2008) Segmentation of heart sounds and heart murmurs. J Mech Med Biol 8: 4.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi