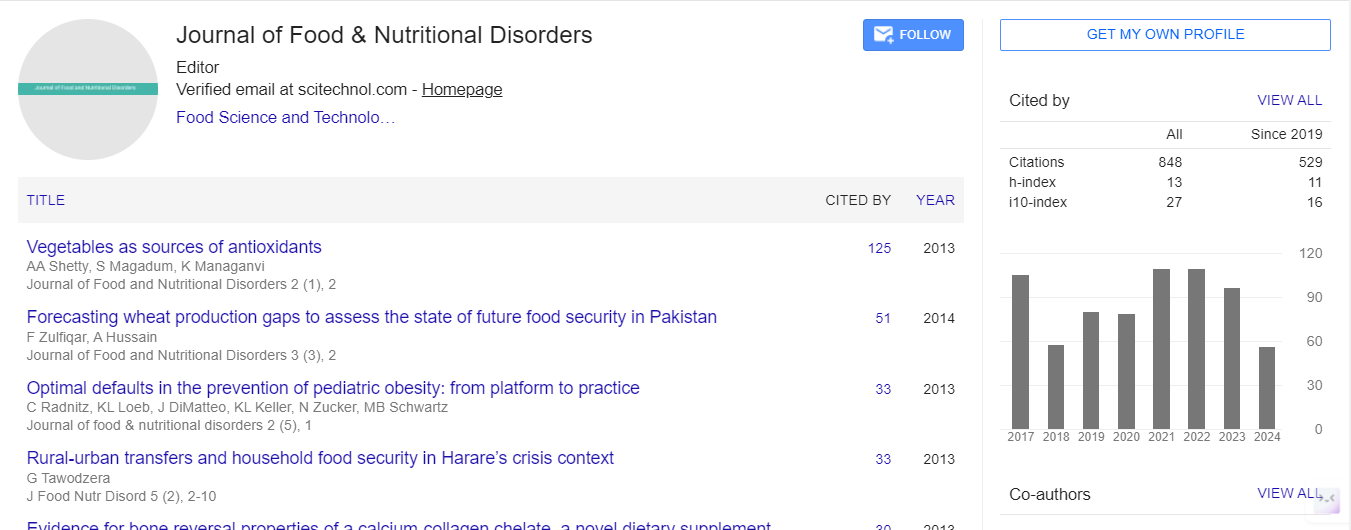
Research Article, J Food Nutr Disor Vol: 7 Issue: 1
Evaluation of the Nutritional Status of Hemodialysate Patients
Olfa Berriche, Nadia Ben Amor*, Faten Mahjoub, Chaima Jemai, Ines Lahmar, Oumayma Samti, Chiraz Amrouch and Henda Jamoussi
Department of Diabetology and Nutritional Diseases, National Institute of Nutrition and Food Technology of Tunisia, Tunisia
*Corresponding Author : Nadia Ben Amor
Resident Doctor in Nutrition, Department of Diabetology and Nutritional Diseases, National Institute of Nutrition and Food Technology, Tunisia
Tel: (+216)98425170
E-mail: bestnadou@yahoo.fr
Received: December 13, 2017 Accepted: January 03, 2018 Published: January 08, 2018
Citation: Berriche O, Amor NB, Lahmar I, Jemaï C Oumayma S, et al. (2018) Evaluation of the Nutritional Status of Hemodialysate Patients. J Food Nutr Disor 7:1. doi: 10.4172/2324-9323.1000242
Abstract
Introduction: Chronic hemodialysis is often malnourished which can impair the effectiveness of dialysis and increases morbidity and mortality. Evaluation of the nutritional status of these patients is difficult and requires the simultaneous use of several parameters. Patients and methods: This cross-sectional study involved 30 patients under the age of 65, followed by the nephrology department of Rabta Hospital in Tunis. These patients were recruited during a month from January to February 2017. The assessment of nutritional status was based on: a food survey, anthropometric measurements (dry weight, height, Body Mass Index, percentage of weight loss within six months, brachial circumference), biological assays (hemogram, C-reactive protein, albuminemia, blood cholesterol) and the Nutritional Risk Index. Results: More than half of our patients had an average daily energy intake <25 kcal/kg/d. Only 6.7% of our patients had satisfactory average daily protein rations. Dietary micronutrient evaluation revealed that our population had insufficient intakes of calcium, iron, vitamins B1 and B9. The frequency of malnutrition varied according to the anthropometric parameter used: 13.3% had a weight loss of more than 10% in the last 6 months, 46.7% had a Body Mass Index <23 kg/m² and 40% had a brachial circumference <22 cm. The albuminemia was <35 g/l in 36.6% of cases. Conclusion: The management of chronic hemodialysis patients must be multidisciplinary: nephrologist, nutritionist and dietician.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi