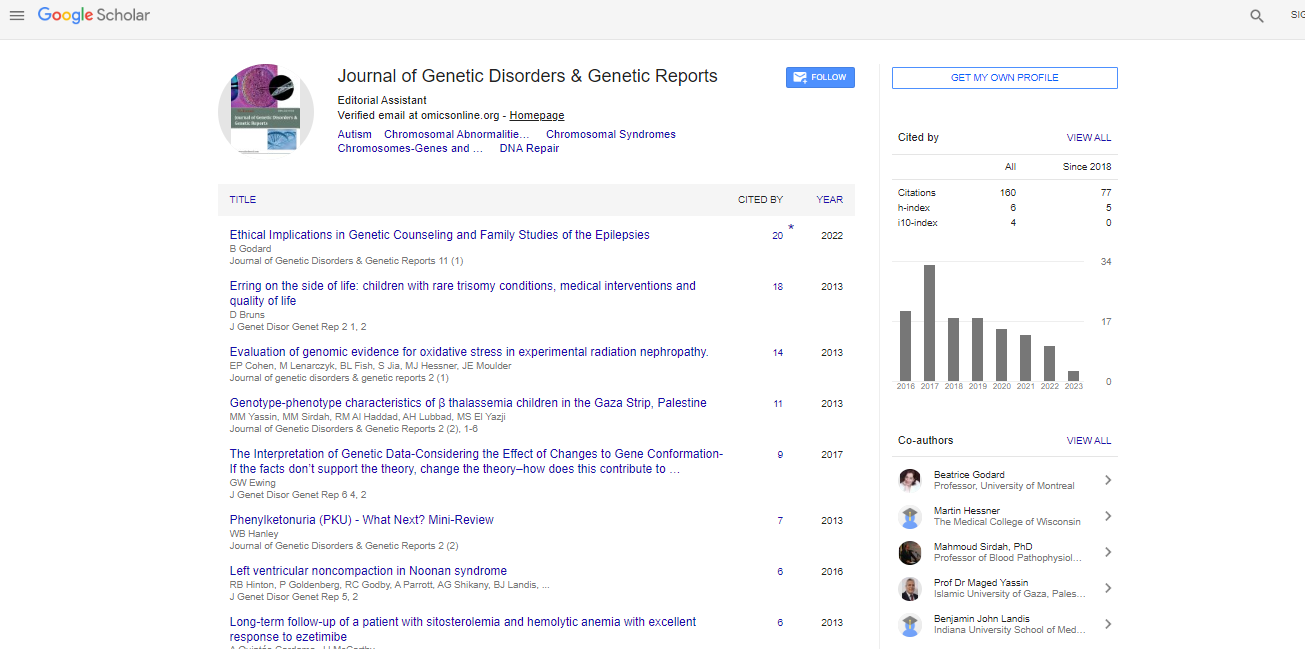
Research Article, J Genet Disor Genet Rep Vol: 7 Issue: 1
Involvement of TLR4 Polymorphisms on Colorectal Cancer Treatment
Omrane I1*, Baroudi O1, Medimegh I1, Ayari H1, Kourda N2, Mezlini A3, Bougatef K1 and Benammar-Elgaaied A1
1Laboratoire de Génétique Immunologie et Pathologie Humaine, Faculté des Sciences de Tunis, Université de Tunis EL MANAR, Tunisie
2Service d’anatomie et de cytologie pathologique de l’Hôpital Charles Nicolle de Tunis, Tunisie
3Service d’oncologie médicale de l’institut Salah Azaiez de Tunis, Tunisie
*Corresponding Author : Inés Omrane
Laboratoire de Génétique I mmunologie et Pathologie Humaine, Faculté des Sciences de Tunis, Université EL MANAR, campus universitaire, Tunis 2092, Tunisie
Tel: +(216) 20618547
E-mail: inesomrane@hotmail.fr
Received: April 05, 2018 Accepted: May 21, 2018 Published: May 28, 2018
Citation: Omrane I, Baroudi O, Medimegh I, Ayari H, Kourda N, et al. (2018) Involvement of TLR4 Polymorphisms on Colorectal Cancer Treatment . J Genet Disor Genet Rep 7:1. doi: 10.4172/2327-5790.1000171
Abstract
The important role of polymorphisms on immunity genes in the susceptibility to various diseases has been widely described. Both polymorphisms D299D and T399I of TLR4 are shown associated with inflammatory bowel diseases as well as colorectal cancer. Previously, we have shown that TLR4 polymorphisms are significantly associated with disease presentation of colorectal cancer such as late stage, differentiation as well as lymph, node and metastasis. Our study aimed to investigate an association between TLR4 D299G and T399I polymorphisms in Tunisian patients with colorectal cancer treatment. We found that T399I and D299G polymorphism of TLR4 were significantly associated with adjuvant chemotherapy and radical surgery. We also showed that mutant alleles of T399I and D299G combined genotypes and haplotypes may affect the effectiveness of therapy. Finally, we showed no significant longer survival and TLR4 polymorphisms. In conclusion, we suggest that polymorphisms in TLR4 gene may be predictive of treatment type.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi