Review Article, J Clin Nutr Metab Vol: 1 Issue: 2
Nutrigenetics of Non-Alcoholic Fatty Liver Disease: What do we know so Far?
Chara Vezou, Ioanna-Panagiota Kalafati and George V Dedoussis*
Department of Dietetics and Nutritional Science, Harokopio University, Athens, Greece
*Corresponding Author : GV Dedoussis
Department of Dietetics and Nutritional Science, School of Health Science and Education, Harokopio University, 70 El Venizelou Ave, 17671, Athens, Greece
Tel: +30 2109549304
E-mail: dedousi@hua.gr
Received: October 03, 2017 Accepted: October 20, 2017 Published: October 27, 2017
Citation: Vezou C, Kalafati I, Dedoussis GV (2017) Nutrigenetics of Non-Alcoholic Fatty Liver Disease: What do we know so far? J Clin Nutr Metab 1:2.
Abstract
Non-alcoholic fatty liver disease (NAFLD) tends to be a new epidemic. It is now considered as the new element of metabolic syndrome, since it is highly correlated with obesity and diabetes mellitus type II. However, there are some patients whose disease is not linked to metabolic abnormalities; the etiology of this type of disease is the genetic background. Main genetic contributors to NAFLD are PNPLA3, TM6SF2 and GCKR. Genetic variations in these loci have been associated with NAFLD onset and progression. Moreover, dietary habits and nutrients’ intake can affect the disease status. Diet composition, such as anti-inflammatory and pro-inflammatory polyunsaturated fatty acids (PUFAs) and carbohydrates intake, along with energy intake constitute key factors in the pathogenesis of NAFLD and development of non-alcoholic steatohepatitis (NASH). Up to now, treatment of NAFLD is based on generalized dietary intervention. However, there is an urgent need for personalized dietary advice in order to provide health professionals with more precise and drastic NAFLD management tools. Nutrigenetics is a field that examines how genetic variation affects response to diet or nutrients. This literature review meets the need of a summary of all available data regarding nutrigenetics of NAFLD. So far, studies in the area are scarce; however, they hold promise for future personalized dietary interventions, aiming to the reduction of NAFLD incidence.
Keywords: NAFLD; Nutrition; Genetics; Nutrigenetics; Fatty liver; NASH
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a public health problem that is prevalent in 20% of the population worldwide [1]. The main pathogenetic factor of NAFLD is the excess deposition of triglycerides in the hepatocytes in absence of other causes of steatosis, including excess alcohol intake and inborn errors of metabolism [2]. The histological classification of the disease varies from simple steatosis to non-alcoholic steatohepatitis (NASH), fibrosis and cirrhosis with its clinical consequences [3]. NAFLD is associated, as an independent risk factor, with metabolic syndrome, type 2 diabetes, cardiovascular disease and chronic kidney disease [4,5]. These associations are summarized in the “multiple hit” hypothesis for the development of the disease [6]. We now know that there are two types of NAFLD patients; those who are genetically predisposed to develop the disease, carrying the I148M variant in PNPLA3 and/or the E167K variant in TM6SF2 and those whose disease is associated with features of metabolic syndrome [7]. Genetically predisposed NAFLD is usually not accompanied with insulin resistance. However, there are many patients who are genetically susceptible to NAFLD but in the same time they have developed metabolic abnormalities.
Dietary habits, environmental and genetic factors can lead to the development of insulin resistance, obesity with adipocyte proliferation and changes in the intestinal microbiome and as a result in the increase of hepatic inflammation [6]. Epidemiological studies, clinical cases, family and twin studies reveal that there are genetic determinants, which significantly contribute in the development of steatosis [8]. It has been now proved that diet composition along with caloric intake can either contribute to the development of NAFLD and NASH or lead to the regression of liver disease [6,9]. However, we now need to explore any gene-diet interactions that can affect the development and progression of NAFLD. Decoding such interactions could be of great use in clinical practice.
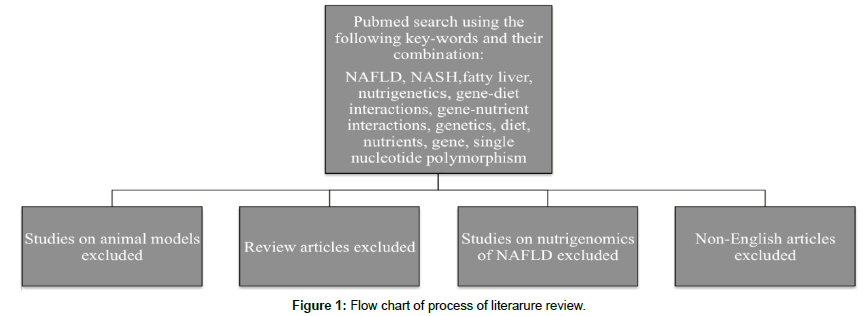
So far, there is very little knowledge about gene-diet interactions of NAFLD. Herein, we summarize the results of published human studies, regarding the nutrigenetics of the disease. Most studies include PNPLA3, the most well studied NAFLD-related gene; however, there are a few studies that refer to GCKR, TM6SF2 or oxidative stress associated genes. Flowchart of the research and studies included in this literature review are summarized in Figure 1 and Table 1, respectively.
| Authors | Year of Publication | Gene(s) studied | Type of Diet/Nutrient involved |
|---|---|---|---|
| Davis et al. [25] | 2010 | PNPLA3 | CHO |
| Sevastianova et al. [26] | 2011 | PNPLA3 | Hypocaloric, low CHO diet |
| Santoro et al. [16] | 2012 | PNPLA3 | PUFAs intake |
| Nobili et al. [21] | 2013 | PNPLA3 | DHA |
| Nobili et al. [27] | 2014 | PNPLA3 | Dietary pattern |
| Scorletti et al. [20] | 2015 | PNPLA3 | EPA + DHA |
| Krawczyk et al. [29] | 2017 | PNPLA3, TM6SF2 | Caloric restriction |
| Kaliora et al. [36] | 2017 | GCKR | Mediterranean Diet |
| Miele et al. [39] | 2014 | GSTT1, CYP1A1, CYP2E1DraI, SULT1A1, GSTM1 | Fruits, grilled meat or fish, alcohol |
Table 1: Studies included in literature review.
PNPLA3
Patatin-like phospholipase-3 (PNPLA3) gene is located on human chromosome 22 and encodes 481 amino acids for making protein adiponutrin which is expressed in fat cells (adipocytes) and liver cells (hepatocytes) [10,11]. It is believed that adiponutrin plays a key role in lipogenesis, acting as an acetyl-CoA-independent transacetylase and in lipolysis, acting as a triglyceride hydrolase [12]. In 2008, it was first reported that a single nucleotide polymorphism at protein position 148 results in substitution of amino acid isoleucine to methionine (I148M, rs738409) and this variant was associated with increased risk of developing NAFLD [11]. Since then, many studies reported the same effect of PNPLA3 variant on NAFLD development and nowadays PNPLA3 rs738409 is considered a risk factor for the disease.
Polyunsaturated fatty acids (PUFAs) have been proved to be associated with the onset and progression of NAFLD [13]. Double blind randomized clinical trials have come to the conclusion that intrahepatic fat content and the risk of developing NASH is significantly reduced when patients are supplemented with omega 3 fatty acids [14]. Their beneficial effect is exerted through their antioxidant and anti-inflammatory properties. However, no optimal dose has been decided yet. On the other hand, omega 6 fatty acids mainly have a pro-inflammatory role [15-17]. Therefore, it is believed that lowering the dietary intake of omega 6/omega 3 PUFAs could hinder several metabolic diseases, including NAFLD [15]. An interaction between PNPLA3 rs738409 variant and dietary ration of omega 6/omega 3 PUFAs has been observed in 127 children and adolescents of various ethnicities (Caucasian, Hispanic and African) [16]. The dietary intake of PUFAs was assessed with 3-day food records and the hepatic fat fraction (%HFF) with abdominal magnetic resonance imaging (MRI). The results indicate that participants homozygous for the minor allele would benefit by a higher consumption of omega 3 fatty acids in order to improve their hepatic fat content and their NAFLD level. The mechanism that underlies these findings is based on the hydrolytic function of PNPLA3 and especially the inhibition of hydrolyzing n-9 fatty acids in presence of rs738409 variant [17]. In human body, omega 6 fatty acids are some of the primary compounds for the synthesis of n-9 fatty acids, which consist the most common fatty acids derived from the diet [18]. The I148M variant increases the cellular accumulation of triglycerides in presence of excess FFAs by significantly down-regulating the triglycerides hydrolysis [19]. It could be speculated that carriers of the rs734809 minor allele tend to increase triglycerides into the liver, while the excess of omega 6 fatty acids not incorporated into triglycerides leads to over-synthesis of pro-inflammatory omega 6 derived species, triggering NASH [16].
On the contrary, a double blind placebo controlled trial in adults showed that after 15-18 months of intervention with supplement of eicosapentanoic acid (EPA) and docosahexaenoic acid (DHA), the I148M/M gene variant of PNPLA3 was independently associated with decreased percentage of DHA tissue enrichment and higher liver fat [20]. In line with the latter study, another randomized controlled trial was conducted in sixty children with NAFLD for 24 months and checked the response of DHA supplementation in association with PNPLA3 I148M variant. Children with the PNPLA3 148M/M genotype had no beneficial effect after DHA supplementation regarding liver fat, and carrying the 148M allele doubled the risk of severe steatosis at the end of the trial [21]. These results clarify that PNPLA3 I148M implicate in omega-3 fatty acids mobilization in the liver, and subjects with the variant have lower level of DHA [16]. Moreover, omega-3 fatty acids decrease the expression of sterol response element binding protein 1c (SREBP1c), a key regulatory factor in hepatic lipogenesis and carriers of the PNPLA3 148M allele are likely to have decreased de novo lipogenesis as a feedback mechanism to avoid excessive lipid accumulation [22]. Thus, it is possible that the lack of response to DHA+EPA treatment in decreasing liver fat percentage in PNPLA3 I148M/M subjects could be due to the fact that these subjects already have low levels of de novo lipogenesis [20].
The majority of published studies indicate an aggravating role of carbohydrates on the accumulation of liver fat [23,24]. Moreover, it is now believed that more important than the quantity of carbohydrates is the quality as simple sugars are mostly implicated in the pathogenesis of the disease. Recently, the scientific interest tends to be focused on clarifying the interaction between carbohydrate intake and genes related to NAFLD. Specifically, in a study of 153 Hispanic children and adolescents, high carbohydrate and high total sugar intake was positively correlated with hepatic fat content, only in carriers of the GG genotype of PNPLA3 rs738409 variant [25]. These findings are supported by the theory that the GG genotype attenuates the capacity of the carriers to hydrolyze triglycerides in the liver, so in presence of excess consumption of high dietary sugar there is an overexpression of PNPLA3 variant and, consequently, severely reduced activity of the enzyme [25].
In another study, 18 subjects underwent a hypocaloric, lowcarbohydrate diet for 6 days and exhibited a greater reduction in liver fat content in PNPLA3 148MM group in comparison with the PNPLA3 148II group [26]. Authors attributed the results to the baseline difference in insulin sensitivity than to the PNPLA3 mutation per se due to the fact that PNPLA3 I148M variant appears to promote intrahepatocellular triglyceride accumulation by either inhibiting triglyceride hydrolysis or promoting de novo lipogenesis [26].
Similarly, in 200 children from Italy a moderate to severe intake of sweetened beverages led to higher liver fat deposition for the carriers of G allele, and a decreased consumption of vegetables declined the risk of severe steatosis in the same carriers [27]. These data are supported by the hypothesis that the effect of the PNPLA3 I148M is intensified by diets rich in carbohydrates, resulting in increased hepatic lipogenesis [25]. It could also be speculated that vegetables represent a source of substrates for hepatic lipogenesis.
The results of the aforementioned studies come in contradiction with a 3-week intervention study in which 16 subjects, 9 homozygous for the minor allele (GG) and 6 homozygous for the major allele (CC), were overfed with simple carbohydrates to conclude that carriers of CC genotype had higher levels of lipogenic index and liver fat content compared to individuals with GG genotype, reinforcing the role of PNPLA3 I148M variant in diminishing hepatic de novo synthesis of triglycerides [28].
Recently, Krawczyk et al. [29] published a 4-month dietary intervention study in 143 NAFLD patients and 180 controls. Dietary intervention included caloric restriction without changes in the physical activity level of the participants. Authors reported that hepatic steatosis and anthropometric traits were statistically significantly improved in carriers of PNPLA3 or TM6SF2 risk allele. However, it was found that the observed improvements were not associated with the genotype of the individuals. The presence of a PNPLA3 or TM6SF2 risk allele was statistically significantly associated with WHR change only. The results of this study indicate that genetic background may not be an irreversible risk factor and that dietary therapy of NAFLD can have beneficial results in all patients.
GCKR
Glucokinase regulatory (GCKR) gene is one of the NAFLDassociated genes that have been identified by genome wide association studies (GWAS) [30]. GCKR gene encodes a protein, which binds to glucokinase (GCK) allosterically and modulates its activity on hepatic glucose metabolism and signs hepatic lipogenesis [31]. Overexpression of GCK results in increase in hepatic glycolytic flux, de novo lipogenesis and triglyceride levels and as a consequence in progress of NAFLD [29]. There are two common variants of GCKR that have been associated with NAFLD and according to several GWAS studies they are in strong linkage disequilibrium (LD) (HapMap CEU r2 = 0.93, CHB r2 = 0.82) [32,33]. One of them is GCKR rs780094, an intronic variant, which firstly associated with NAFLD disease by a GWAS study that consisted of 592 diagnosed by biopsy NAFLD patients from the NASH Clinical Research Network [31], and the second one is GCKR rs1260326, a non-synonymous GCKR variant, which is characterized by a C to T substitution encoding a proline-to-leucine substitution at amino acid position 446 (P446L) [33]. The P446L variant acts as a competitive inhibitor in glucokinase’s response to fructose-6-phosphate, thereby determining constitutive activation of hepatic glucose uptake [34]. This leads to decreased circulating fasting glucose and insulin levels, but on the other hand it would lead to increased glycolysis and the production of malonyl-CoA which favors hepatic fat accumulation by serving as a substrate for lipogenesis and by blocking fatty acid oxidation [31,35].
There are several studies that investigate the interaction between GCKR variants and diet in pathogenesis of lipogenesis, but only one that examines the effect of nutritional counseling and GCKR rs1260326 variant in patients with diagnosed NAFLD [36]. In this single-arm prospective intervention trial 44 Caucasian individuals with NAFLD diagnosed by abdominal ultrasound and shear wave elastography/fibroscan underwent a 6-month diet monitoring in order to achieve a reduction up to 5% of their initial body weight. The dietary intervention included the following elements: 30% of total energy from fat (<10% as SFAs, ~10% as MUFAs and ~10% as PUFAs), 20% as protein, 50% as carbohydrates, 300 mg/day as dietary cholesterol and 20-30 g fibers/day. The sample divided into two groups according to the GCKR rs1260326 genotype, the T-allele carriers and the non T-allele carriers. At the end of 6 months, the risk allele was associated with lower glucose blood levels and higher oxLDL as a result of nutritional counseling. These findings could be supported by the proxy SNP of rs1260326, rs780094 [32]. The GCRK rs1260326 variant participates in inducing hepatic glucose uptake, in enhancement of glycolysis and production of malonyl-CoA, which in its turn is involved in the inhibition of carnitine-palmitoyl tranferase-1 and as a consequence fatty acid oxidation. In mitochondria, β-oxidation is reduced and enhancement of triglyceride accumulation occurs. Authors suggested that the cumulative effect of extra-mitochondrial fatty acid oxidation potentially increases ROS generation, oxidative damage and mitochondrial impairment Table 1 [36-38].
Other genes
The first reported nutrigenetic study regarding NAFLD was conducted by Miele et al. [39]. Authors examined the interaction of dietary and lifestyle factors with oxidative stress associated genes in 294 Italian NAFLD patients and 359 controls. Results showed that the consumption of more than two fruits per day interacts with the risk allele of variants of the following genes: glutathione S-transferase Mu 1 (GSTM1), glutathione S-transferase theta 1 (GSTT1), CYP1A1 and CYP2E1DraI of the cytochrome P450 superfamily, and sulfotransferase 1A1 (SULT1A1). This interaction was positively associated with the risk of developing NAFLD. Similar results were reported for the carriers of GSTM1, GSTT1, CYP1A1, and SULTI1A1 variants when consumption of grilled meat or fish was higher than once per week. This result indicates a possible role of aromatic hydrocarbons in liver steatosis. Another interesting finding was that carriers of the CYP2E1*5B allele who consume a moderate intake of alcohol (<20 g/day for females, <30 g/day for males) have 75% lower odds of developing NAFLD. Furthermore, this Italian study was the first to report a gene-gene interaction for NAFLD.
Conclusion
The current literature review summarizes the results of studies, which have focused on the different response of individuals to diet according to their genetic background regarding NAFLD. Omega 3 fatty acids and carbohydrates seem to be the main dietary factors that interact with NAFLD-associated genes and alter their main effect on the disease. However, the field of nutrigenetics of NAFLD is scarce and preliminary and there are only a handful of studies published on this field, yet promising. More studies are necessary in order to decode these gene-diet pathways and to “move” research towards the personalized nutritional therapy of NAFLD.
Acknowledgements
IP Kalafati and GV Dedoussis were funded by “Research Project for Excellence ΙΚΥ/SIEMENS”.
References
- Bellentani S (2017) The epidemiology of non-alcoholic fatty liver disease. Liver Int 37: 81-84.
- Banini BA, Sanyal AJ (2016) Nonalcoholic Fatty Liver Disease: Epidemiology, Pathogenesis, Natural History, Diagnosis, and Current Treatment Options. Clin Med Insights Ther 8: 75-84.
- Chalasani N, Yunossi Z, Lavine JE, Diehl AM, Brunt EM, et al. (2012) The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 55: 2005-2023.
- Bang KB, Cho YK (2015) Comorbidities and Metabolic Derangement of NAFLD. J Lifestyle Med 5: 7-13.
- Mikolasevic I, Milic S, Turk Wensveen T, Grgic I, Jakopcic I, et al. (2016) Nonalcoholic fatty liver disease - A multisystem disease? World J Gastroenterol 22: 9488-9505.
- Buzzetti E, Pinzani M, Tsochatzis EA (2016) The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 65: 1038-1048.
- Petäjä E, Yki-Järvinen H (2016) Definitions of Normal Liver Fat and the Association of Insulin Sensitivity with Acquired and Genetic NAFLD—A Systematic Review. Int J Mol Sci 17: 633.
- Dongiovanni P, Valenti L (2016) Genetics of nonalcoholic fatty liver disease. Metabolism 65: 1026-1037.
- Romero-Gómez M, Zelber-Sagi S, Trenell M (2017). Treatment of NAFLD with diet, physical activity and exercise. J Hepatol 67: 829-846.
- Kotronen A, Johansson LE, Johansson LM, Roos C, Westerbacka J, et al. (2009) A common variant in PNPLA3, which encodes adiponutrin, is associated with liver fat content in humans. Diabetologia 52: 1056-1060.
- Romeo S, Kozlitina J, Xing C, Pertsemlidis A, Cox D, et al. (2008) Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 40:1461-1465.
- Naik A, Košir R, Rozman D (2013) Genomic aspects of NAFLD pathogenesis. Genomics 102: 84-95.
- Mouzaki M, Allard JP (2012) The role of nutrients in the development, progression, and treatment of nonalcoholic fatty liver disease. J Clin Gastroenterol 46: 457-467.
- Parker HM, Johnson NA, Burdon CA, Cohn JS, O'Connor HT, George J (2012) Omega-3 supplementation and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol 56: 944-951.
- Enos R, Velázquez K, McClellan J, Cranford T (2015) Lowering the dietary omega-6: omega-3 does not hinder nonalcoholic fatty-liver disease development in a murine model. Nutrition Research 35: 449-459.
- Santoro N, Savoye M, Kim G, Marotto K, Shaw MM, et al. (2012) Hepatic fat accumulation is modulated by the interaction between the rs738409 variant in the PNPLA3 gene and the dietary omega6/omega3 PUFA intake. PLoS ONE 7: e3782.
- Huang Y, Cohen JC, Hobbs HH (2011) Expression and characterization of a PNPLA3 protein isoform (I148M) associated with nonalcoholic fatty liver disease. J Biol Chem 286: 37085-37093.
- Simopoulos AP (2008) The Importance of the Omega6/Omega3 Fatty Acids Ratio in Cardiovascular Disease and Other Chronic Diseases. Exp Biol Med 233: 674-678.
- Perttilä J, Huaman-Samanez C, Caron S, Tanhuanpää K, Staels B, et al. (2012) PNPLA3 is Regulated by Glucose in Human Hepatocytes and its I148M Mutant Slows Down Triglyceride Hydrolysis. Am J Physiol Endocrinol Metab 302: E1063-1069.
- Scorletti E, West AL, Bhatia L, Hoile SP, McCormick KG, et al. (2015) Treating liver fat and serum triglyceride levels in NAFLD, effects of PNPLA3 and TM6SF2 genotypes: Results from the WELCOME trial. J Hepatol 63: 1476-1483.
- Nobili V, Bedogni G, Donati B, Alisi A, Valenti L (2013) The I148M variant of PNPLA3 reduces the response to docosahexaenoic acid in children with non-alcoholic fatty liver disease. J Med Food 16: 957-960.
- Mancina RM, Matikainen N, Maglio C, Soderlund S, Lundbom N, et al. (2015) Paradoxical dissociation between hepatic fat content and de novo lipogenesis due to PNPLA3 sequence variant. J Clin Endocrinol. Metab 100: E821-E825.
- Maersk M, Belza A, Stødkilde-Jørgensen H, Ringgaard S, Chabanova E, et al. (2012) Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr 95: 283-289.
- Neuschwander-Tetri BA (2013) Carbohydrate intake and nonalcoholic fatty liver disease. Curr Opin Clin Nutr 16: 446-452.
- Davis JN, Le KA, Walker RW, Vikman S, Spruijt-Metz D, et al. (2010) Increased hepatic fat in overweight Hispanic youth influenced by interaction between genetic variation in PNPLA3 and high dietary carbohydrate and sugar consumption. Am J Clin Nutr 92: 1522-1527.
- Sevastianova K, Kotronen A, Gastaldelli A, Perttila J, Hakkarainen A, et al. (2011) Genetic variation in PNPLA3 (adiponutrin) confers sensitivity to weight loss-induced decrease in liver fat in humans. Am J Clin Nutr 94: 104-111.
- Nobili V, Liccardo D, Bedogni G, Salvatori G, Gnani D, et al. (2014) Influence of dietary pattern, physical activity, and I148M PNPLA3 on steatosis severity in at-risk adolescents. Genes Nutr 9: 392.
- Sevastianova K, Santos A, Kotronen A, Hakkarainen A, Makkonen J, et al. (2012) Effect of short-term carbohydrate overfeeding and long-term weight loss on liver fat in overweight humans. Am J Clin Nutr 96: 727-734.
- Kaliora M, Rau M, Schattenberg JM, Bantel H, Pathil A, et al. (2017) Combined effects of the PNPLA3 rs738409, TM6SF2 rs58542926, and MBOAT7 rs641738 variants on NAFLD severity: a multicenter biopsy-based study. J Lipid Res 58: 247-255.
- Speliotes EK, Yerges-Armstrong LM, Wu J, Hernaez R, Kim LJ, et al. (2011) Genome-wide association analysis identifies variants associated with nonalcoholic fatty liver disease that have distinct effects on metabolic traits. PLoS Genet 7: e1001324.
- Peter A, Stefan N, Cegan A, Walenta M, Wagner S, et al. (2011) Hepatic glucokinase expression is associated with lipogenesis and fatty liver in humans. J Clin Endocrinol Metab 96: E1126-1130.
- Diabetes Genetics Initiative of Broad Institute of Harvard and MIT, Lund University, and Novartis Institutes of BioMedical Research, Saxena R, Voight BF, Lyssenko V, Burtt NP, et al. (2007) Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316: 1331-1336.
- Sparso T, Andersen G, Nielsen T, Burgdorf KS, Gjesing AP, et al. (2008) The GCKR rs780094 polymorphism is associated with elevated fasting serum triacylglycerol, reduced fasting and OGTT-related insulinaemia, and reduced risk of type 2 diabetes. Diabetologia 51: 70-75.
- Beer NL, Tribble ND, McCulloch LJ, Roos C, Johnson PR, et al. (2009) The P446L variant in GCKR associated with fasting plasma glucose and triglyceride levels exerts its effect through increased glucokinase activity in liver. Hum Mol Genet 18: 4081-4088.
- Rametta R, Mozzi E, Dongiovanni P, Motta BM, Milano M, et al. (2013) Increased insulin receptor substrate 2 expression is associated with steatohepatitis and altered lipid metabolism in obese subjects. Int J Obesity 37: 986-992.
- Kaliora AC, Kalafati IP, Gioxari A, Diolintzi A, Kokkinos A, et al. (2017) A modified response of NAFLD patients with non significant fibrosis in nutritional counseling according to GCKR rs1260326. Doi: 10.1007/s00394-017-1499-7.
- Lieber CS (2004) CYP2E1: from ASH to NASH. Hepatol Res 28: 1-11.
- Anstee QM, Goldin RD (2006) Mouse models in non-alcoholic fatty liver disease and steatohepatitis research. Int J Exp Pathol 87: 1-16.
- Miele L, Dall’Armi V, Cefalo C, Nedovic B, Arzani D, et al. (2014) A case-control study on the effect of metabolic gene polymorphisms, nutrition, and their interaction on the risk of non-alcoholic fatty liver disease. Genes Nutr 9: 383.
 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi